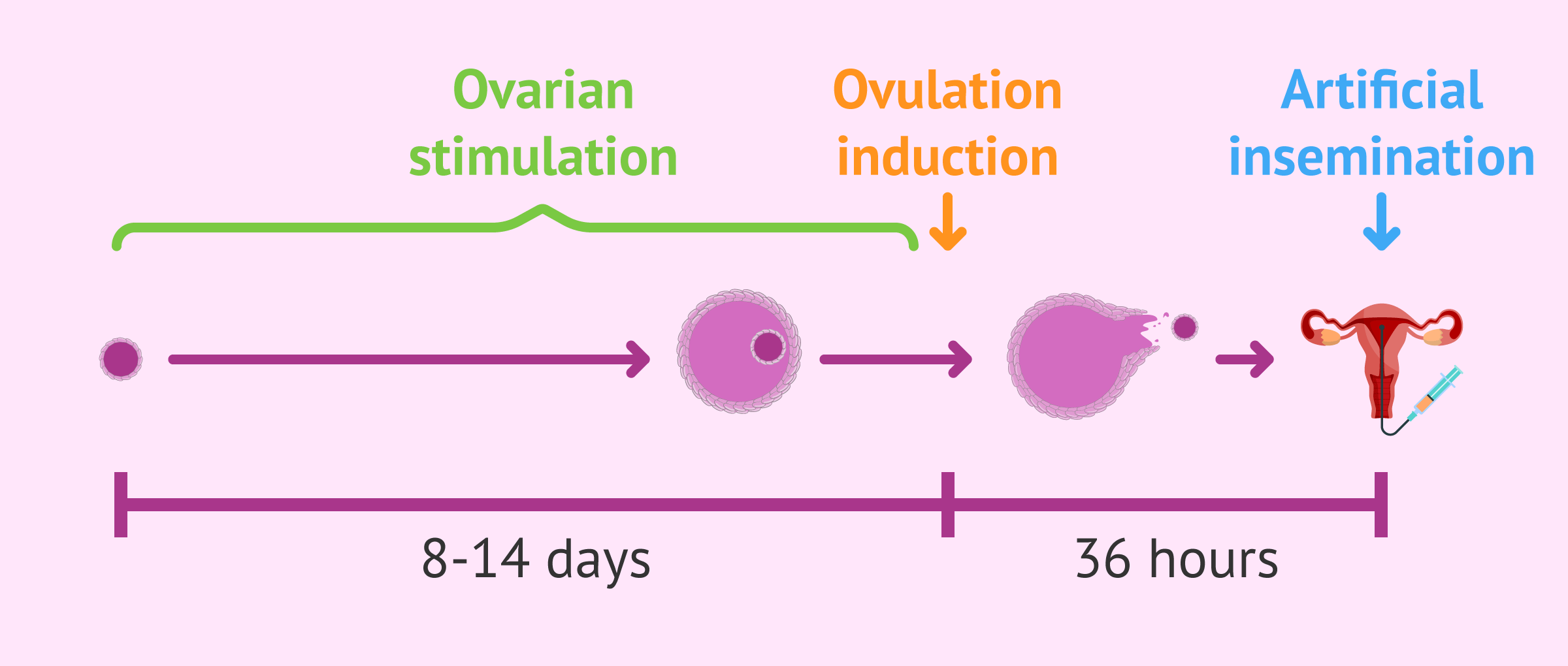
In an artificial insemination (AI) process, it is necessary to perform controlled ovarian stimulation to allow follicular development and ovulation of one or two mature eggs.
This is achieved through hormonal medication in lower doses than those used for in vitro fertilization (IVF). The drugs used have various trade names and the vast majority contain gonadotropins such as FSH and LH or compounds such as clomiphene citrate.
The guidelines for administering hormone medication depend on the characteristics of each patient and can be modified as treatment progresses and ultrasound checks are performed.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 5.6.
- 5.7.
- 6.
- 7.
- 8.
What is controlled ovarian stimulation?
In a normal menstrual cycle, a woman develops a follicle in her ovary inside which an egg grows. At the time of ovulation, the egg is released into the fallopian tubes, where it encounters the sperm and fertilization takes place.
Fertility specialists aim to control the menstrual cycle in such a way as to ensure the maturation of one or more eggs. In addition, ovulation is induced at a specific time to coincide with insemination with the male's semen.
Therefore, artificial insemination treatment consists of two parts in which the drugs used are different:
- Controlled ovulation induction
- exogenous menstrual cycle hormones (FSH and LH) are administered to trigger follicular development.
- Ovulation induction
- the hCG hormone induces ovulation 36 hours after it is injected. At this time artificial intrauterine insemination is performed.
For AI, the sperm used can be from the woman's partner or from an anonymous donor. In both cases, sperm capacitation will be done to prepare the semen before it is introduced into the uterus.
Dosage and days of treatment
The goal of AI stimulation is to achieve one or at most two mature eggs that can be fertilized in the tubes. Therefore, ovarian stimulation is gentle compared to that done in IVF, where multiple follicular development is intended.
The hormone doses in an AI are low and are administered by injections that the woman gives herself according to medical advice.
The stimulation process usually lasts between 8 and 14 days. The injections start on day 2 or 3 of the beginning of the menstrual cycle, taking as the beginning of the cycle the day that menstruation arrives.
The gynecologist observes the maturation process of the follicles with periodic transvaginal ultrasounds and blood estradiol analysis.
The monitoring of the stimulation aims to control the number of follicles in each of the ovaries, schedule the time of insemination and measure the thickness of the endometrium.
The follicles have to reach 18 millimeters in diameter, at which time the hCG hormone is administered to trigger ovulation.
In case the follicular development does not take place as expected, the gynecologist can modify the hormonal dose and/or the days of treatment.
Patient Characteristics
Several aspects are taken into account to determine the most appropriate medication pattern for each woman, of which we highlight:
- Patient Characteristics
- Morphology of the ovaries
- Body mass
- Hormone analysis
- Response to stimulation in previous cycles
In assisted reproduction, it is not possible to standardize the process of ovarian stimulation, but it is necessary to make a personalized treatment for each patient.
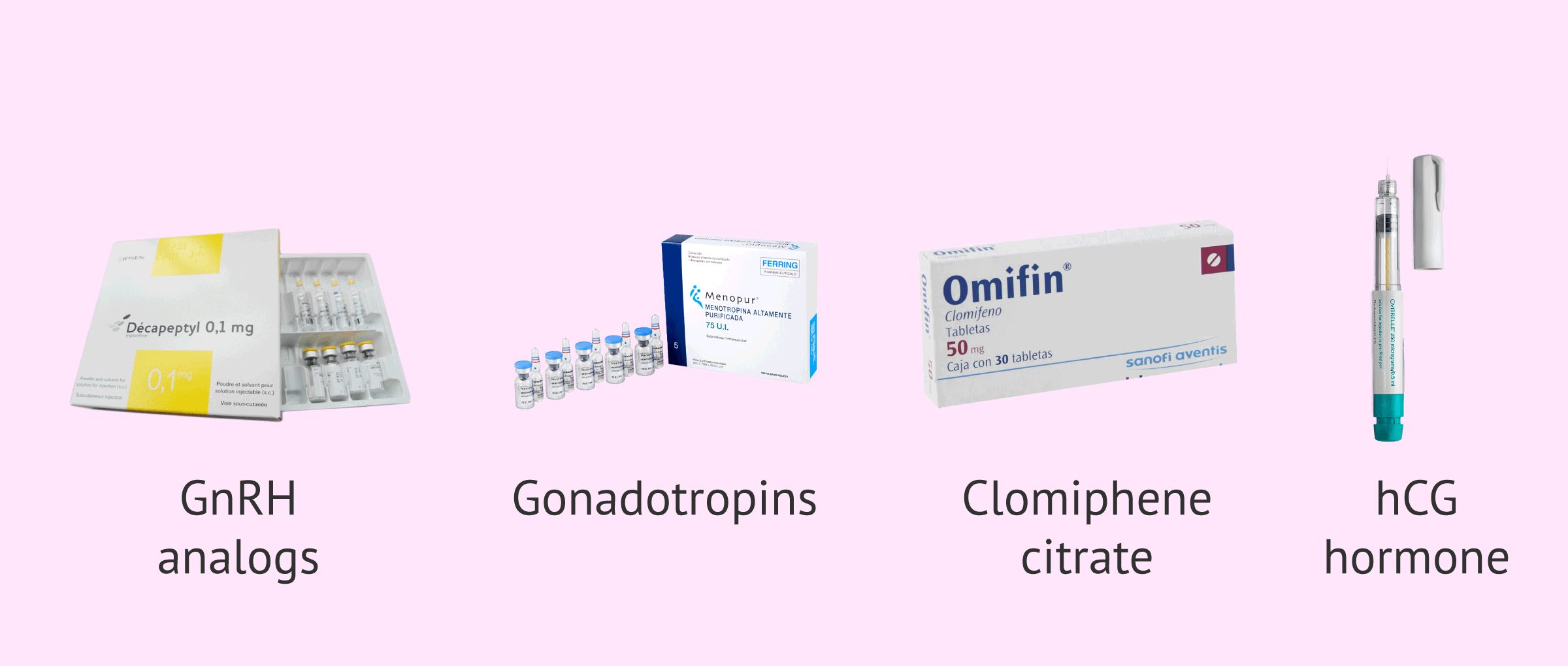
Medication for artificial insemination
The types of drugs for controlled ovarian stimulation in AI are diverse and have different mechanisms of action. In addition, each type of drug has many brand names with very different prices.
Below, we will comment on the most used ones today:
- GnRH analogues
- serve for ovarian suppression, that is, they inhibit the endogenous sex hormones of the menstrual cycle. They can be applied with a short or a long treatment and the most used are Cetrotide, Procrin, Decapeptyl and Orgalutran.
- Gonadotropins
- These are the exogenous hormones that cause follicular development itself and those that must be administered in low doses. The drugs that contain them are Gonal, Menopur and Puregon among others.
- Clomiphene citrate
- is used in women with ovulatory problems such as polycystic ovary syndrome (PCOS). It stimulates follicular development and also causes ovulation. One of the most widely used drugs is Omifin.
- Hormone hCG
- consists of a single injection given 34-36 hours before AI to induce ovulation. The most famous drug is Ovitrelle.
It should be noted that all of these drugs must be used under medical supervision infertility treatment.
Did you know that we can help you to choose a fertility clinic for your IUI cycle? All you have to do is get your Fertility Report now. It is an easy-to-use tool that is capable of filtering the best clinics and tailor an individual report exclusively for you with useful tips that will help you make a well informed decision.
Risks of controlled ovarian stimulation
The main drawback that can arise from hormonal medication in an AI is ovarian hyperstimulation syndrome (OHSS).
OHSS occurs when the ovaries respond abnormally highly to the hormones used in stimulation. This can lead to increased permeability of blood vessels and promote the accumulation of fluid in the peritoneal cavity of the abdomen, which causes great pain.
The risk of suffering this symptom in an artificial insemination treatment is low since the stimulation is very mild. In addition, the monitoring and control carried out makes it possible to anticipate a high response and therefore to stop the medication pattern before this alteration takes place.
Other disadvantages of controlled ovarian stimulation are the side effects it causes, such as abdominal swelling, headache, breast discomfort, etc. However, these pass in a few days and are of no great importance.
FAQs from users
Is it possible to predict the response to ovarian stimulation in AI?
The response of the ovaries to ovarian stimulation can be predicted by parameters that indicate what a woman's ovarian reserve is like at a given moment: the follicle count in the ovaries by transvaginal ultrasound and the anti-Müllerian hormone (AMH) value; these data, as well as the body mass index, help us to adapt the doses of medication that each woman will need to obtain the most ideal ovarian response.
In an artificial insemination (AI) treatment we look for the growth of one or two follicles, unlike in vitro fertilization (IVF) treatment, in which we look for the growth of all the antral follicles present in the ovaries. Therefore, in an artificial insemination we usually perform a very gentle ovarian stimulation, with low doses of gonadotropins, and most often the vast majority of women (both those with a high ovarian reserve and those with normal or low ovarian reserve) respond in a very similar way, with one or two follicles.
In the case of women with polycystic ovaries there are occasions in which the ovarian response is greater, and a greater number of follicles may grow and the treatment must be cancelled in these cases due to the risk of multiple pregnancies. In women with polycystic ovaries we usually start the treatment with an even lower dose of gonadotropins, or even with a pattern of administration every 36 hours instead of the usual 24 hours, in order to reduce as much as possible the response of the ovaries and minimize the possibility of cancellation of the cycle.
Does an ovarian stimulation treatment bring forward menopause?
No, ovarian stimulation causes follicles to grow that would not naturally grow, but it does not accelerate the rate of follicle or egg loss.
In a woman's normal cycle, a follicle is selected to be the one chosen for ovulation. Along with that selected follicle, a cohort of follicles that are not chosen will be lost after ovulation.
In ovarian stimulation, this cohort of pre-selected follicles is used so that they grow and more eggs can be obtained than are produced naturally and thus have a greater yield of the assisted reproduction technique.
How many days does ovarian stimulation last in an artificial insemination?
Although it depends on the type of cycles a woman has and her response to ovarian stimulation, it is usually 10-12 days.
At what point does the dominant follicle reach a size of about 17 mm?
In artificial insemination (AI) it is important to know the ideal moment to perform the insemination, that is, to place the semen in the uterus.
For this it is essential to do ultrasound controls to control the size of the follicle. In the case of elongated follicles, two diameter measurements are always taken to see the real size of the follicle in order to know at what moment to induce the ovulation externally, with the administration of ovitrelle.
The moment when the dominant follicle reaches about 17 mm is usually on day 9 of the stimulation cycle, but there are women who reach the size of 17 before or after. That is why it is so important to do ultrasound controls every 48 hours.
Is there a risk of multiple pregnancy using artificial insemination?
With ovarian stimulation, the number of eggs that can be fertilized by sperm is increased in order to increase the probability of pregnancy. Therefore, there is a greater risk of multiple pregnancy compared to what happens in a natural cycle.
To reduce this risk, it is important that ovarian stimulation is moderate, preventing the development and ovulation of more follicles than desired.
Is letrozole used for ovarian stimulation?
Letrozole is a drug that increases the secretion of GnRH in the brain and this causes the release of more FSH and LH. Therefore, it does cause a stimulation in the ovary.
This type of drug, like clomiphene citrate, is used in women with anovulatory problems in both artificial insemination and scheduled intercourse. In both cases, it is necessary to inject Ovitrelle to trigger ovulation.
What is the ovarian stimulation protocol for AI?
Ovarian stimulation for artificial insemination (AI) is minimal. This means that it uses low doses of hormonal drugs, unlike in vitro fertilization (IVF).
Its explanation is based on the fact that in an AI treatment only one or two ovarian follicles at the most are intended to develop. Therefore, the amounts of hormones to be administered to the patient during ovarian stimulation will be lower.
The patient will be administered gonadotropins for 10-12 days and when the follicles are of adequate size, the woman will be placed on hCG. At this time, the physician will plan the insemination in a maximum of 34 hours, to avoid ovulation.
Recommended reading
If you want to know what medications are used for ovarian induction, we recommend you this post: What medications are used for ovarian stimulation?
For more information about artificial insemination and what the treatment consists of, you can access our specialized page on this subject: What is intrauterine artificial insemination?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Farquhar C, Liu E, Armstrong S, Arroll N, Lensen S, Brown J. Intrauterine insemination with ovarian stimulation versus expectant management for unexplained infertility (TUI): a pragmatic, open-label, randomised, controlled, two-centre trial. Lancet. 2018 Feb 3;391(10119):441-450. doi: 10.1016/S0140-6736(17)32406-6. Epub 2017 Nov 23.
Galiiano D. Ovarian stimulation, insemination, and contraception. Fertil Steril. 2016 Mar;105(3):607. doi: 10.1016/j.fertnstert.2015.12.025. Epub 2016 Jan 8.
Liu J, Li TC, Wang J, Wang W, Hou Z, Liu J. The impact of ovarian stimulation on the outcome of intrauterine insemination treatment: an analysis of 8893 cycles. BJOG. 2016 Sep;123 Suppl 3:70-5. doi: 10.1111/1471-0528.14020.
Yildirim G, Turkgeldi LS, Koroglu N, Mervetalmac S. Predictive factors for pregnancy outcome following controlled ovarian stimulation and intrauterine insemination. J Pak Med Assoc
. 2017 Mar;67(3):422-427.
FAQs from users: 'Is it possible to predict the response to ovarian stimulation in AI?', 'Does an ovarian stimulation treatment bring forward menopause?', 'How many days does ovarian stimulation last in an artificial insemination?', 'At what point does the dominant follicle reach a size of about 17 mm?', 'Is there a risk of multiple pregnancy using artificial insemination?', 'Is letrozole used for ovarian stimulation?' and 'What is the ovarian stimulation protocol for AI?'.
Authors and contributors

More information about Michelle Lorraine Embleton
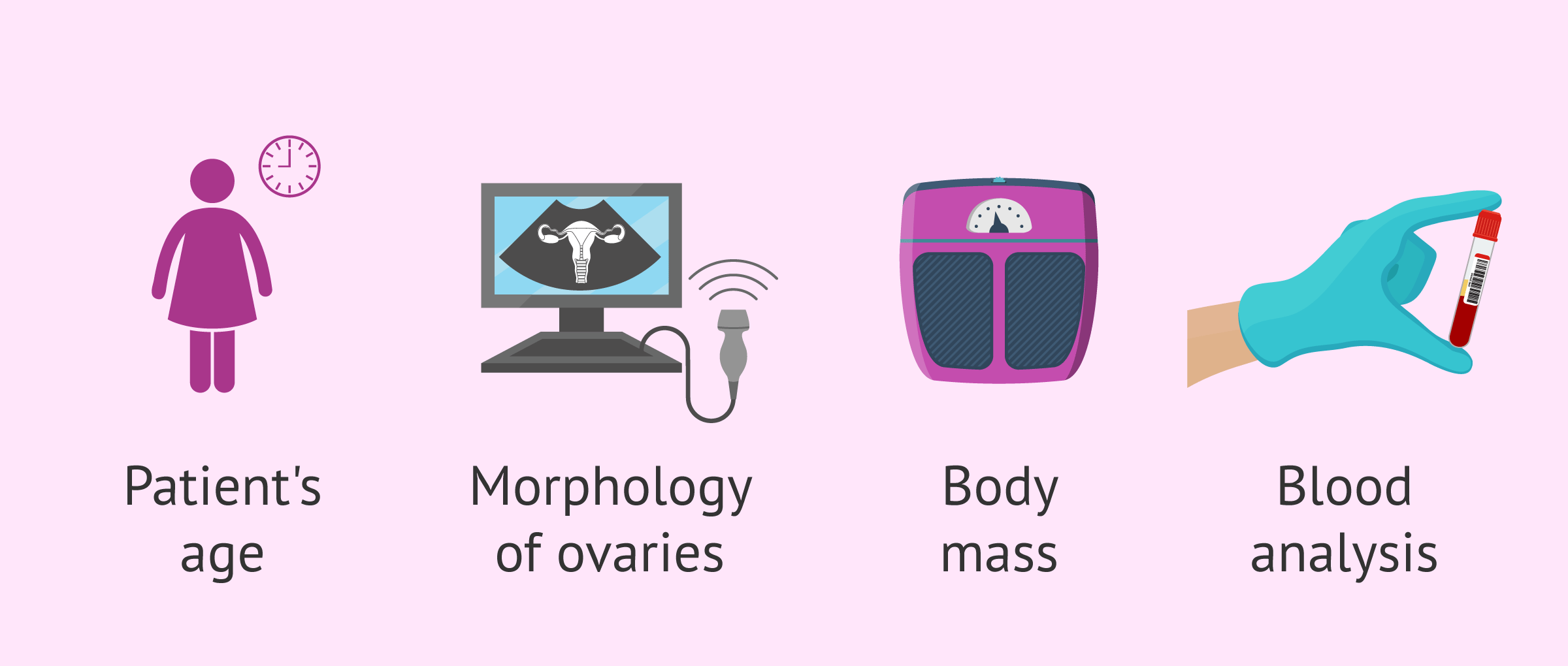






Are the medications used for ovulation induction always the same for every patient?
Hi Nela,
No. Everyone is different and not all women respond equally to medication. Therefore, to determine the most appropriate medication regimen for each woman, it is necessary to take into account her age, the morphology of her ovaries, her weight, her hormone levels, or whether she has had previous cycles.
Therefore, it is of vital importance that each person has a personalized treatment to achieve higher success rates in the treatments.
This post might be interesting for you: What medications are used for ovarian induction?
Hope this clarifies your question.
Best
Hi, I’m on AI treatment. I started a few weeks ago and after 6 injections of Menopur 75 my gynaecologist told me that I had to stop treatment because of the risk of multiple pregnancy as there were too many follicles. To start the treatment again I have to wait two periods to eliminate the eggs generated with the medication. Is it normal to have to wait two periods? Also, he told me that I am going to start with delayed ovulation AI treatment. Does anyone know what this is? I hope someone can clarify it for me and good luck!
Hi, I’m Dina, I started ovulation induction this month. Last year they gave me the same treatment and I was hyper-stimulated, they did a laparoscopy and at two months naturally and without looking for it at that time I got pregnant, at 9 and a half weeks I had a miscarriage. This was devastating for my husband and me, this month exactly a year ago we found out that we were pregnant, and coincidentally this month we started treatment, I am very nervous and very afraid, but I also have all the hopes that everything will be fine. Anyway, my question is: what is the probability of getting pregnant through ovulation induction? And what happens if this method does not work?