Endoscopy is a technique that involves inserting a tube attached to a camera (endoscope) to view the inside of an organ or cavity. This instrument is inserted through a small incision or through natural openings such as the vagina or anus.
Until recently, such procedures were used for diagnostic purposes only. However, nowadays, endoscopic methods also allow a correct treatment of pathologies in a less aggressive way.
Gynecological endoscopy does not require hospitalization, allowing the patient to return home the same day of the intervention. Within it, two modalities can be distinguished: hysteroscopy and laparoscopy.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 4.6.
- 4.7.
- 5.
- 6.
- 7.
What is endoscopy?
Endoscopy is a diagnostic procedure that involves introducing an optical system or endoscope through a natural hole or a small incision to view the inside of an organ or cavity. In this way, information is obtained that cannot be reliably provided by other external techniques such as an X-ray. This is a surgical procedure that is performed under local or regional anesthesia or sedation.
An endoscope is an instrument made up of a lighted tube that is inserted into cavities or ducts for viewing.
Gynecological endoscopic surgery is a novel discipline with two purposes: diagnosis and treatment of pathologies. In this case, to visualize the cavities of the female reproductive organs, the endoscope can be inserted in two ways:
- Through the vagina (hysteroscopy).
- Through small incisions in the abdomen (laparoscopy).
The decision whether to perform a hysteroscopy or a laparoscopy will be made by the specialist depending on the characteristics of each patient or the situation itself.
Advantages of endoscopic surgery
Endoscopic surgery is considered the technique of choice in certain situations due to its many advantages:
- Rapid recovery.
- Hospitalization for a few hours.
- Smaller scars.
- Less chance of bleeding and blood loss.
- There is communication between the patient and the doctor during the test if the woman is not sedated.
Because of the above mentioned characteristics, endoscopic techniques are known as minimally invasive surgery.
Gynecological hysteroscopy
Hysteroscopy is a technique that consists of diagnosing and treating pathologies of the uterine cavity through direct visualization. A small hysteroscope (3-5 mm) is inserted through the opening of the cervix. In addition, carbon dioxide or physiological serum must be injected to dilate the cavity.
The hysteroscope is a thin gynecological instrument that can be rigid, semi-rigid, or flexible.
There are two types of hysteroscopy depending on their purpose and the thickness of the hysteroscope: diagnostic and surgical. In both types, the woman lies in gynecological position. The doctor then places the speculum to widen the opening of the vagina and cleans the cervix with an iodine solution.
Once the area has been cleaned, the doctor gently inserts the hysteroscope through the cervix, releasing fluid to dilate the area, which will help to clearly see the uterine cavity. By using monitors, the specialist will examine the uterus in detail. In addition, if the procedure is performed to treat a pathology, it will insert other instruments through the hysteroscope.
Below we will list each type of hysteroscopy.
Diagnostic hysteroscopy
In this hysteroscopy model, a smaller calibre hysteroscope is used and is carried out on an outpatient basis, without the need for anesthesia or sedation.
The best time to perform hysteroscopy in patients of childbearing age is in the proliferative phase of the menstrual cycle, that is, between the sixth and tenth day. This reduces bleeding and the endometrium is thinner.
Diagnostic hysteroscopy is indicated in the following cases:
- When uterine adhesions, endometrial polyps, myomas or uterine septa are suspected.
- When IUD and other devices are removed.
- In infertility studies and implantation failures.
- Evaluation of menstrual alterations.
- Evaluation of the endometrial cavity.
The use of this technique ensures good reliability in the interpretation of images, minimizing, in turn, the risk of complications. However, secondary discomfort such as pelvic or abdominal pain may occur.
Surgical hysteroscopy
This hysteroscopy model is performed when there is a diagnosis of any endometrial or uterine alteration.
In surgical hysteroscopy, the hysteroscope is thicker and is performed in the operating room under sedation or regional anesthesia.
In addition, the hysteroscope is equipped with gynecological tools to perform different types of surgery, whether it is necessary to remove or manipulate. Apart from that, when a surgical hysteroscopy is performed, it is necessary to dilate the cervix more than in a diagnostic hysteroscopy.
The cases in which surgical hysteroscopy is indicated are described below:
- Endometrial ablation or reduction.
- Removal of fibroids or polyps.
- Elimination of intrauterine adhesions.
- Resection of uterine septa.
Apart from these situations in which a hysteroscopy is advisable, it should not be forgotten that it is also a useful procedure in case of a fertility study.
Risks
Thanks to technological advances, hysteroscopy has become a primary technique in gynecological practice.
Generally speaking, hysteroscopy is considered a safe technique, so the likelihood of complications is low, but not impossible. There is a minimal chance of perforation of the uterus, which can lead to bleeding.
Other complications of hysteroscopy are discussed below:
- Reflex syncope: due to a lack of skill of the specialist and the diameter of the hysteroscope. This complication usually causes discomfort, a feeling of warmth, pallor, etc.
- Gas embolism: it is very serious, but uncommon. This is a side effect of carbon dioxide distension.
- Pelvic infection.
It is therefore vitally important to detect any signs of a complication in order to avoid putting women's health at risk.
Contraindications of hysteroscopy
Although hysteroscopy is one of the main techniques in gynecology, there are cases where it should not be performed. Some of them are described below:
- Women in acute phase of pelvic infection, as it can cause endometrial or tubal dissemination.
- Excessive uterine bleeding because it would prevent a correct visualization of the area.
- Cervical Cancer.
- Evolutionary gestation.
As an exception, hysteroscopy may be performed on a pregnant woman to remove an IUD, provided it happens before the 10th pregnancy week.
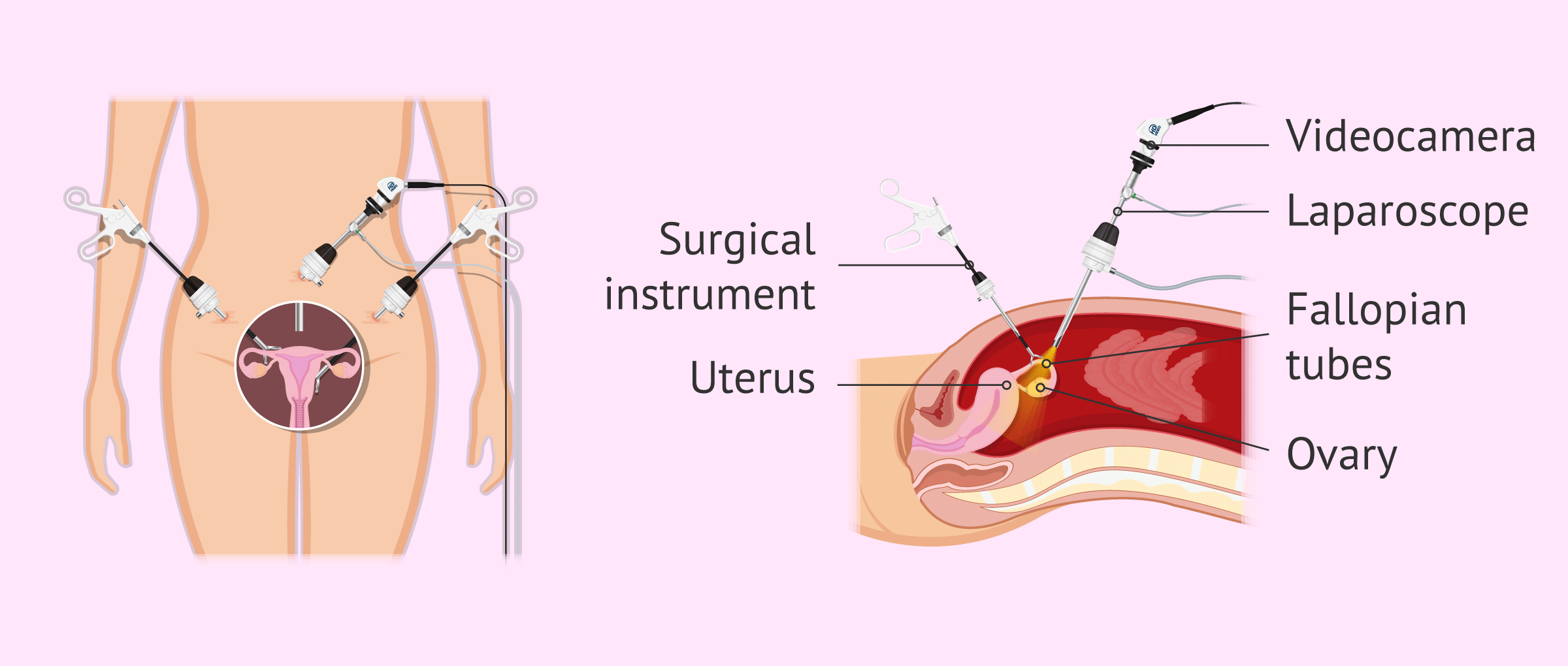
Gynecological laparoscopy
Laparoscopy is a surgical procedure to look for problems in the abdomen or female reproductive system (uterus, fallopian tubes, and ovaries). A thin tube (laparoscope) is inserted through a small incision in the navel. This is a minimally invasive technique, so the patient can return to her day-to-day routine in 72-78 hours.
Gynecologic laparoscopy requires the patient to fast and take a laxative the day before surgery to have empty bowels.
Like in hysteroscopy, there are two simultaneous objectives of laparoscopy: On the one hand, this test aims to diagnose and on the other hand solve all those problems that are detected during the intervention.
Diagnostic laparoscopy
This is a procedure whose recovery is quick and causes little pain. The practice of laparoscopy for diagnostic purposes is indicated when there are suspicions of endometriosis, sterility, bleeding from the ovaries and pain in the abdomen and pelvis area, for which no explanation can be found.
The timing of the diagnostic laparoscopy will always depend on the purpose and the specialist's own opinion.
Surgical Laparoscopy
Today, surgical laparoscopy is a fairly safe surgical model for treating gynaecological pathologies. To do this, the doctor will make small incisions through which he will introduce a trocar in order to be able to use the surgical tools, such as scissors, tweezers, etc.
This procedure is performed under general anesthesia, so women won’t feel pain during the procedure. The surgery of most gynecological alterations can be performed by laparoscopy. Below, we well discuss the main indications for surgical laparoscopy:
- Removal of ovarian cysts of fibroids.
- Treatment of endometriosis.
- Removal of ectopic pregnancy.
- Hysterectomy or womb removal.
When a patient is undergoing surgical laparoscopy, she should take preoperative antibiotics to reduce the risk of infection.
Recovery
The recovery of a woman who undergoes laparoscopy is fast and is usually accompanied by the administration of some pain relievers.
Another aspect that can modify the recovery is the use of carbon dioxide for better visualization, as this gas can cause discomfort in the abdomen during the first days after surgery. This is completely normal and symptoms will disappear as carbon dioxide is absorbed.
As for sexual activity, a woman may have sex once any bleeding has stopped.
Risks of laparoscopy
Like any surgery, laparoscopy may cause some complications. Common risks include bleeding at the site of insertion or misadministration of gas for visualization.
Other risks of gynecological laparoscopy are:
- Damage to the inside of the stomach, intestine, bladder, or ureters.
- Adverse reaction to anesthesia.
- Blood clots
- Abdominal swelling.
In spite of this, there is usually no danger to the woman's health during laparoscopy since it is a fairly safe technique.
FAQs from users
What are the risks of hysteroscopy before IVF?
Hysteroscopy is a minimally invasive procedure for diagnostic and therapeutic use in the management of various intrauterine and intracervical gynecological pathologies. It is indicated in assisted reproduction treatments (endometrial polyps, uterine malformations, endometrial scars, submucous myomas, implantation failure, etc.).
However, despite being a minimally invasive and very safe procedure, it is not exempt from complications like any other surgery. Fortunately, these complications occur in a very low percentage.
Therefore, the fact of performing a hysteroscopy prior to performing an IVF cycle, whenever indicated, can increase the rate of gestation, implantation and evolutionary pregnancy.
Can a uterine fibroid be removed by laparoscopy?
Yes, in qualified hands, the laparoscopic approach may be used to remove subserosal and intramural uterine fibroids.
However, the fibroids most related to reproductive problems are submucosal fibroids, which are removed by hysteroscopy.
Read more
Can hysteroscopy be performed while on period?
No. Hysteroscopy is usually performed in the proliferative phase of the menstrual cycle, although it could be performed at any stage of the cycle in which the patient is not bleeding and there is no possibility of pregnancy.
Does gynecological hysteroscopy hurt?
Normally, diagnostic hysteroscopy is not painful, but after the procedure there may be discomfort similar to that of a period.
In cases where a surgical hysteroscopy is performed, there is no pain because it is performed under anesthesia.
What are recommendations for post-hysteroscopy?
Generally speaking, the patient should avoid bathing but may take a shower. In addition, sexual intercourse is not advised for approximately two weeks.
It is not necessary to stay in bed, but it is necessary to have some rest during the first 24 hours.
If you have abdominal discomfort similar to that of your period, you may take some pain medication.
Is hysteroscopy and hysterosonography the same thing?
No. Hysteroscopy and hysterosonography are two different tests.
Hysteroscopy consists of inserting a tube (hysteroscope) attached to a camera through the cervix; while hysterosonography is a transvaginal ultrasound that is performed along with the insertion of saline through the cervix by means of a cannula.
How is the recovery from a laparoscopy?
When a woman undergoes a laparoscopy, it is recommended that she does not take heavy objects and that she avoids physical exertion. It is normal to maintain these measures for about two weeks.
In addition, it is advisable to follow a balanced diet, although avoiding the consumption of fats and spicy foods.
Suggested for you
Women who struggle to conceive due to uterus problems will be recommended to perform a gynecological endoscopy. You can read more about this in the following article: Uterine Factor Infertility- Diagnosis, Characteristics & Treatment.
Hysteroscopy is also one of the tests performed to assess a woman's fertility. You can get more information about other complementary techniques in the following article: Female Fertility Tests - How Do You Know If You Can't Get Pregnant?
If you want to get the permeability of your fallopian tubes checked, have a look at: How Is a Hysterosalpingography (HSG) Performed?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Alonso L, Carugno J. Chronic Endometritis: Three-dimensional Ultrasound and Hysteroscopy Correlation. J Minim Invasive Gynecol. 2019 Sep 3. pii: S1553-4650(19)30406-6. doi: 10.1016/j.jmig.2019.08.028
Guzmán G, Zaldivar A, Garza P, Bustos H H. Complicaciones en laparoscopia ginecológica. Perinatol Reprod Hum 2000; 14: 32-47 (View)
Joo J, Moon HK, Moon YE. Identification of predictors for acute postoperative pain after gynecological laparoscopy. Medicine (Baltimore). 2019 Oct;98(42):e17621. doi: 10.1097/MD.0000000000017621 (View)
Kamath MS, Bosteels J, D'Hooghe TM, Seshadri S, Weyers S, Mol BWJ, Broekmans FJ, Sunkara SK. Cochrane Database Syst Rev. 2019 Apr 16;4:CD012856. doi: 10.1002/14651858
Luthra N, Namrata, Grewal A. Air embolism following hysteroscopy. J Anaesthesiol Clin Pharmacol. 2019 Jul-Sep;35(3):416-417. doi: 10.4103/joacp.JOACP_143_18 (View)
Rodríguez-Mias NL, Cubo-Abert M, Gomila-Villalonga L, Gómez-Cabeza J, Poza-Barrasús JL, Gil-Moreno A. Hysteroscopic myomectomy without anesthesia. Obstet Gynecol Sci. 2019 May;62(3):183-185. doi: 10.5468/ogs.2019.62.3.183 (View)
Sánchez C, Brito, M. Histeroscopia diagnóstica y terapéutica. Experiencia de 10 años. Rev Obstet Ginecol Venez v.66 n.4 Caracas dic. 2006 (View)
Smorgick N, Rabinovitch I, Levinsohn-Tavor O, Maymon R, Vaknin Z, Pansky M. Two-step hysteroscopy for management of morbidly adherent retained products of conception. Arch Gynecol Obstet. 2019 Sep;300(3):669-674. doi: 10.1007/s00404-019-05246-1
Tsunoda Y, Matsushima T, Yoneyama K, Takeshita T. Role of hysteroscopy in the diagnosis of uterine artery pseudoaneurysm: a case report. J Obstet Gynaecol. 2019 Oct 14:1-2. doi: 10.1080/01443615.2019.1650261
Utida GM, Kulak J Jr. Hysteroscopic and aspiration biopsies in the histologic evaluation of the endometrium, a comparative study. Medicine (Baltimore). 2019 Oct;98(40):e17183. doi: 10.1097/MD.0000000000017183 (View)
FAQs from users: 'What are the risks of hysteroscopy before IVF?', 'Can a uterine fibroid be removed by laparoscopy?', 'Can hysteroscopy be performed while on period?', 'Does gynecological hysteroscopy hurt?', 'What are recommendations for post-hysteroscopy?', 'Is hysteroscopy and hysterosonography the same thing?' and 'How is the recovery from a laparoscopy?'.