ICSI is a procedure used for in vitro fertilization (IVF) whereby a sperm cell is microinjected directly into an egg to create viable embryos. After that, the resulting embryos are transferred back to the uterus of the intended mother, so that pregnancy hopefully occurs. Given that it is a type of IVF, we often refer to it with the name IVF/ICSI.
The main advantage of ICSI are its high success rates. In most cases, pregnancy is achieved after the first attempt, even in the most severe cases of male infertility.
The fact that it is a type of IVF, with each one of the steps involved, makes the cost of the treatment ranges between $13,000 and $15,000.
Provided below is an index with the 11 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 3.5.
- 3.6.
- 4.
- 4.1.
- 5.
- 6.
- 7.
- 8.
- 8.1.
- 8.2.
- 8.3.
- 8.4.
- 8.5.
- 8.6.
- 8.7.
- 8.8.
- 9.
- 10.
- 11.
Definition
ICSI is the abbreviation of Intracytoplasmic Sperm Injection. This technique allows us to choose the best sperm to insert it inside a microinjection needle.
Then, while the oocyte is being held from one side, the needle is carefully inserted in the opposite side, so that the sperm is injected into the cytoplasm of the egg.
The goal is that the egg and sperm fuse together. In other words, that fertilization takes place successfully.
Therefore, to perform the IVF-ICSI technique only the same amount of sperm is needed as the number of eggs to be fertilized. For this reason, it is the technique of choice when fertility problems are due to a sperm factor in the male.
Difference between IVF & ICSI
The main difference between Intrauterine Insemination (IUI) and IVF is that, in the case of IUI, fertilization occurs inside the woman. In other words, retrieving the eggs is not required. Conversely, in the case of IVF, the eggs are collected prior to being fertilized in the lab. Finally, out of the resulting embryos, the one with the highest quality is selected to be transferred back to the uterus.
ICSI and conventional IVF are similar infertility treatments which differ in the way the sperm is inserted inside the oocyte. In the case of conventional IVF, it is the sperm cell which penetrates the egg coat by itself:
- Classical IVF
- The sperm itself has to go through the egg coat in order to fertilize it.
- ICSI
- The specialist inserts directly the sperm cell into the egg cell. This is what makes it more challenging than classical IVF.
Another major difference between them is related to the cost of each: the more technically challenging, the higher the cost, and ICSI is a great example of this.
Related content: IVF vs. ICSI, Which One Is Better? - How to Make the Right Choice.
As Dr. Miguel Dolz, OB/GYN specialized in Reproductive Medicine, confirms, actually the most widely used IVF technique used if ICSI, especially in countries where the use of reproductive technologies is vastly extended. Simply put, nearly 80% of the clinics use ICSI on a regular basis.
However, he is also in favor of conventional IVF as a more "ecological" alternative. Indeed, classical IVF is less aggressive with the gametes and embryos than other procedures like ICSI.
When is ICSI performed?
When ICSI was first introduced, it was a revolution in the treatment of severe male factor sterility. In these situations, sperm microinjection is indicated because this is the most effective therapeutic option for these patients.
However, ICSI is also chosen by many couples who resort to IVF with the aim of ensuring that fertilization occurs correctly, despite not having a severe male factor.
Assisted procreation, as any other medical treatment, requires that you rely on the professionalism of the doctors and staff of the clinic you choose. Obviously, each clinic is different. Get now your Fertility Report, which will select several clinics for you out of the pool of clinics that meet our strict quality criteria. Moreover, it will offer you a comparison between the fees and conditions each clinic offers in order for you to make a well informed choice.
The following are some of the most important indications for IVF-ICSI.
Azoospermia
This male fertility problem occurs when the sperm count in the ejaculate is zero. There exist two types of azoospermia:
- Obstructive azoospermia: The sperms are prevented from mixing with the remaining seminal fluid due to a blockage in any of the ejaculatory ducts. Sperm production occurs, yet the sperms are not expelled.
- Non-obstructive azoospermia: No sperm is produced, as the problem remains in the testes, which is the location where spermatozoa are created.
For this reason, natural pregnancy is not possible when a man is diagnosed with azoospermia. IVF-ICSI will be the best option in this case, since a large number of sperm is not needed, simply the same as the eggs to be fertilized.
You can continue reading more in detail about this topic in the following article: What is azoospermia? - Causes, diagnosis, and treatment
Oligozoospermia
Oligozoospermia, also known as oligospermia, refers to poor sperm quality caused by the absence of sperm concentration in the ejaculate. The WHO (World Health Organization) uses a cut-off of not less than 15 million sperm per milliliter as a general recommendation or a total concentration of more than 39 million sperm.
There are different degrees of oligospermia; the further away from the reference value, the more severe it is. In the most serious cases, we speak of cryptospermia or cryptozoospermia, which refers to concentrations of sperm below 100,000 spermatozoa/ml of semen.
If you are interested in reading more about this seminal alteration, you can click on this link: What is oligospermia? - Causes, types and treatments
Asthenozoospermia
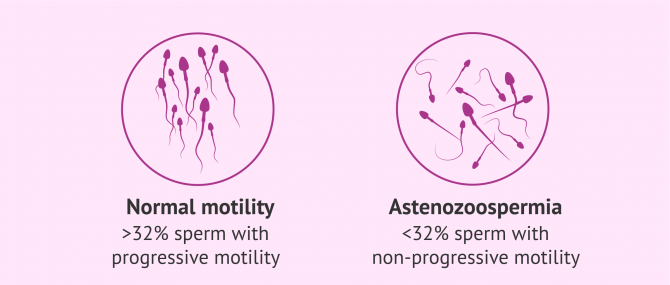
Also known as asthenospermia, this parameter measures sperm quality according to how motile they are. In accordance with the WHO, this pathology is diagnosed whenever the amount of progressive spermatozoa or able to move forward is less than 32%.
Furthermore, the sperm sample is diagnosed as asthenozoopermia if the total count of motile sperms (progressive or non-progressive movement) is lower than 40%.
You can read more about asthenozoospermia in our article: What is asthenozoospermia?
Teratozoospermia
Teratozoospermia or teratospermia refers to a problem in sperm morphology. According to the Kruger strict criteria, the presence of more than 85% abnormal sperm in the ejaculate indicates male sterility. In these cases, ICSI is the most advisable treatment to achieve parenthood.
If the WHO's criteria are followed, then a semen sample is considered to have teratozoospermia if more than 96% of sperm are morphologically abnormal.
Deformities in the shape of the sperm can cause alterations in the movements, the capacity to penetrate the egg, or even give rise to embryos with genetic alterations.
If you would like more information about this seminal alteration, we recommend you visit the following article: What Is Teratozoospermia? - Causes, Types and Treatments.
A combination of abnormal sperm test values
In addition to the above-listed sperm pathologies, it is possible for various sperm values to appear altered in the semen analysis.
Taking this into account, the following combinations are possible:
- Oligoasthenozoospermia: alterations in sperm concentration and motility.
- Oligoteratospermia: alterations in sperm concentration and morphology.
- Asthenoteratospermia: alterations in sperm motility and morphology.
- Oligoasthenoteratospermia: alterations in sperm motility, morphology and concentration.
It is therefore possible to detect several altered semen parameters in the same sperm sample.
Other indications
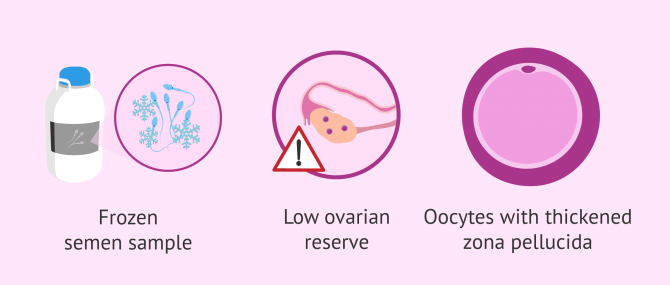
ICSI is also advisable after a vasectomy or in males diagnosed with an infectious disease (HIV, hepatitis, etc.).
Males who have had their semen cryopreserved due to cancer treatments (radiotherapy or chemotherapy) or those unable to ejaculate under normal conditions are recommended to undergo ICSI as well.
ICSI is not so common in cases of female infertility. It is used in cases where a scarce number of oocytes have been obtained after ovum pick-up if there is an enlargement of the zona pellucida, or in women producing poor-quality eggs.
Nevertheless, this is a controversial issue. Many specialists argue that, in cases where the eggs are more fragile, classical IVF is more advisable because the level of manipulation of the eggs is less aggressive.
If you want to know when ICSI is performed, have a look at this link: How Do I Know When ICSI Is Necessary?
How does ICSI work step by step?
The steps to follow in an ICSI procedure are the same as in IVF, but differ in the way the eggs are inseminated:
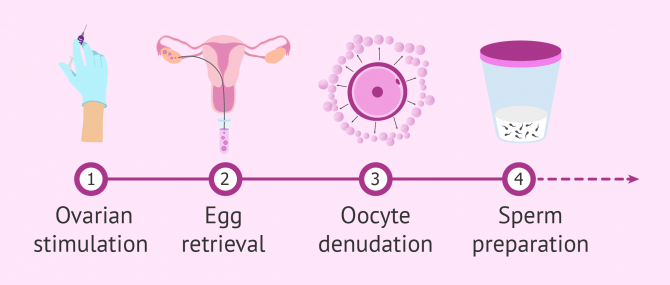
- Controlled ovarian stimulation (COS): Patients are given hormone fertility medications to promote the maturation of multiple egg cells with good quality in a single cycle. Regular ultrasound monitoring is necessary to assess follicle growth.
- Ovum pick-up or follicular puncture: When ultrasounds show the follicles have almost reached the right size for ovulation, egg collection is scheduled. It is a simple surgical procedure that is done with mild anesthesia and takes around 30 minutes. During this process, the follicular fluid (FF) containing the eggs is aspirated.
- Oocyte denudation: It is done at the laboratory and consists in examining the FF obtained after egg harvesting in search of oocytes. After some time resting, the eggs are "stripped", which is to say, the cumulus cells surrounding them are removed.
- Sperm collection and preparation: The semen sample is generally obtained by masturbation and washed prior to fertilization. The washing process is known as sperm capacitation and involves "mixing" only those sperms with the highest quality. When collection cannot be done by means of masturbation, sperms can be obtained through testicular biopsy or epididymal aspiration.
- Egg insemination: A sperm is selected, aspirated with a microinjection needle, and injected into the ovum. The ultimate goal is to ensure that the fusion between both partners' DNAs (i.e. fertilization) occurs.
- Embryo culture: After fertilization, the resulting embryos are cultured in an incubator so that they continue developing. IVF incubators keep the optimum conditions of temperature, light and humidity for embryo growth.
- Preparation of the uterine lining: Estrogens and progesterone are administered through vaginal, mouth or patch route to get her uterine lining to be receptive and in excellent conditions for embryo development.
- Embryo transfer (ET): The best embryo(s) is selected for the transfer according to its quality. ET is a simple step that takes only a few minutes, and anesthesia/sedation is not required. The embryos are placed in the uterine fundus with a fine catheter, so that they are hopefully able to implant to the endometrial lining and lead to a successful pregnancy.
- Embryo freezing: High-quality unused embryos are cryopreserved (frozen) for later use.
Would you like to know all the steps of this treatment in more detail? Don't miss out on this post: ICSI - the process step by step.
Additional techniques
Often, additional services may be required in addition to ICSI-IVF in order to make pregnancy possible or increase the success rates, including:
- IVF/ICSI with testicular biopsy
- In patients with azoospermia, sperm could be retrieved directly from the testes with a testicular biopsy. ICSI is the only technique that can be subsequently used for fertilization.
- pICSI (physiological ICSI)
- The specialist selects those sperm cells that are more likely to fertilize in natural conditions, that is, as in natural conception.
- IMSI
- It stands for Intracytoplasmic Morphologically Selected Sperm Injection. IMSI allows us to select the sperms with the best morphology using high magnification.
- ICSI with Annexin V Columns (MACS)
- To select sperms with the highest quality (non-apoptotic spermatozoa).
- IVF/ICSI with PGD
- Thanks to PGD (Preimplantation Genetic Diagnosis), we can select the embryos that are healthy (free from genetic diseases).
- Assisted Hatching
- This involves weakening the zona pellucida (ZP) of the embryos to facilitate implantation. It is, however, falling into disuse in most laboratories today.
Success rates
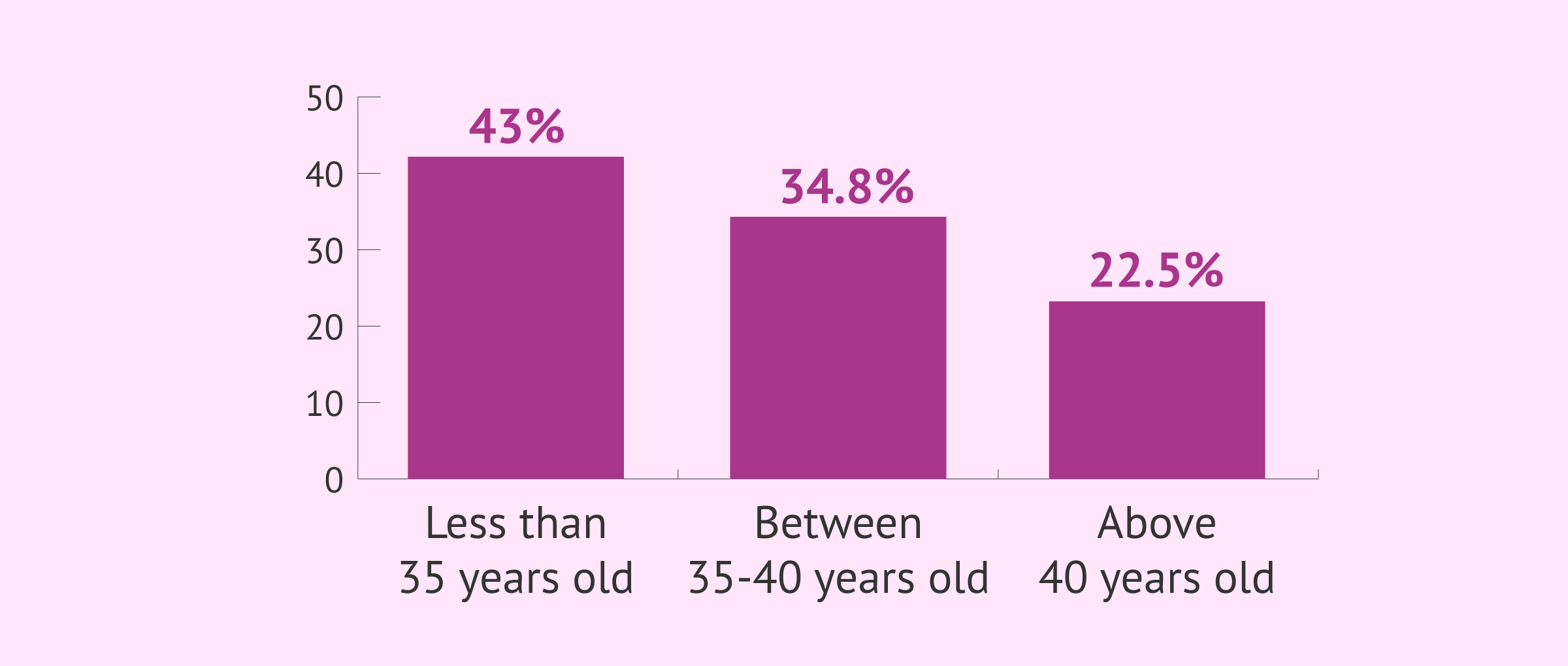
The probability of success of this technique varies according to each particular case. Although there are many factors that can influence the pregnancy rate through IVF, the age of the woman undergoing the treatment is one of the most influential.
The rates of gestation by transfer published in the latest 2022 statistical registry of the Spanish Fertility Society (SEF) according to age are as follows:
- 43.7% in women under 35 years of age.
- 35.0% in women between 35 and 39 years old.
- 21.2% in women over 40 years of age.
However, the pregnancy and delivery rates are not the same, since in some cases gestation does not go to term.
Furthermore, it should not be forgotten that these rates are very general and that they can change not only depending on the case of sterility of each patient, but also on the reproductive center where the treatment is performed.
What is used as a reference also matters when it comes to talking about success rates. For instance, while some consider it has been successful after obtaining a positive pregnancy test (fertilization rate), others refer to the live birth rate solely. This is the reason why one should pay special attention when comparing the success rates of infertility treatments.
You may also enjoy some further information reading this: How Successful Is IVF with ICSI? – Pregnancy & Live Birth Rates.
What are the potential risks and side effects?
The potential risks associated with ICSI include:
- Ovarian Hyperstimulation Syndrome (OHSS): It is due to an excessive response to hormone therapy for ovarian stimulation. It can cause the woman to feel physical discomfort, bloating, etc. However, today it occurs rarely and with a low degree of severity in the vast majority of cases. Ultrasound monitoring is crucial while on ovulation induction for this reason.
- Multiple births: With two-embryo transfers, the probability of having twins reaches 6%. When three embryos are transferred, the probability of having twins rises to 12%, and the likelihood of having triplets to 3%. Current research focuses on improving the embryo selection process to choose only those with excellent quality. This means they aim to improve the success rate with single embryo transfers (SET).
- Miscarriage: It is estimated that miscarriage occurs in 20-22% of the cycles. It usually happens while the woman is on the earliest stages of pregnancy.
- Ectopic pregnancy: It occurs when the embryo implants in a location outside the uterus. Statistical data has shown that 2 to 5 women per every 100 undergoing in vitro fertilization can have an ectopic pregnancy. Chances drop to 1-1.5% in the case of natural pregnancies.
In short, the risks of IVF-ICSI are the same as in classic IVF.
Learn more: What Are the Risks of In Vitro Fertilization (IVF)?
What is the cost of ICSI?
Like any other fertility treatment, the prices of IVF with ICSI are variable and can range between different figures depending on the clinic, country, and particularities of each infertility case.
Special features such as the use of donor eggs and donor sperm or the need for PGD (preimplantation genetic diagnosis) or a testicular biopsy, etc. can increase or decrease the overall cost of ICSI.
Broadly speaking, the cost of ICSI ranges from $13,000 to $15,000. Normally, there is no difference between the fees for conventional IVF and those of ICSI procedures. However, some clinics may offer different prices depending on the method they use for egg fertilization.
Normally, the costs of this fertility treatment don't include stimulation medication which is why it is of utmost importance to inform oneself before starting the process. The cost of this hormonal medication will vary depending on the protocol indicated by the doctor and the necessary doses. However, the general costs for fertility medication are situated between $2,000-5,000.
If you need to undergo IVF to become a mother, we recommend that you generate your Fertility Report now. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Another aspect to keep in mind when estimating the cost of ICSI is related to the personal situation the couple or individual is living currently. While it can work on the first attempt, sometimes it fails, in which case more cycles would be necessary. So, it should be taken into account that costs can vary depending on the severity of the infertility problem and the number of attempts needed.
FAQs from users
In which cases is ICSI used automatically?
ICSI or Intracytoplasmic Sperm Injection is a type of In Vitro Fertilization that is used to fertilize the egg cell. With ICSI, the sperm cell is selected and injected within each one of the eggs collected.
Unanimously recognized indications of ICSI include:
- Severe male infertility: a single sperm per egg cell is enough
- Previous fertilization failure using conventional IVF
- Issues with the oocytes: poor-quality eggs may compromise sperm penetration into the egg cell
- Techniques that involve isolating the egg from the cells that surround it (egg donation, preimplantation diagnosis...)
What are the advantages and disadvantages of ICSI over IVF?
Both techniques are reproductive technologies, and as such, we cannot say that one is better than the other. Actually, it depends on the diagnosis of each couple.
In the case of conventional IVF, we put the oocyte in contact with a determined concentration of sperm, so that the sperm itself fertilizes the egg, which resembles natural fertilization to a large extent.
In many cases, sperm quality is altered, in which case using the sperm won't be possible. In such situations, we use ICSI. It consists in microinjecting the sperm, which is subjectively selected by the embryologists, into the oocyte.
What are the risks of ICSI treatment for the patient?
The most frequent complication is multiple pregnancy determined by the development of multiple follicles in intrauterine insemination (IUI) and the transfer of 2 or more embryos in in-vitro fertilization (IVF).
Ovarian hyperstimulation syndrome is a less frequent but potentially serious complication for which we detail prevention and clinical management strategies. In addition, complications arising from follicular aspiration such as hemorrhage and infection, among others, are discussed.
However, thanks to the development of new pharmacological and laboratory technologies, assisted reproductive procedures are performed within a framework of ample safety.
What are the pros and cons of ICSI over IVF?
ICSI, intracytoplasmic sperm injection was developed in 1988 as a treatment for male infertility, i.e., men with very poor sperm parameters, to treat failure of fertilization with IVF. ICSI is now used routinely in many IVF programs as the fertilization rate is higher than with standard fertilization techniques and the pregnancy rates are higher. There is inadequate information about a possible increase in congenital anomalies with ICSI. There appears to be an increased risk of identical twinning with ICSI, especially with transferring blastocysts. This may be as high as 2%.
When PGD/PGS is required, what is better, ICSI or IVF?
If PGD (preimplantation genetic diagnosis) is to be used as well, egg fertilization is done via ICSI to avoid harmful interferences with PGD outcomes.
In IVF procedures, a percentage of the sperms that tried to penetrate the egg remain adhered to its surface. As a result, some of their genetic material could be incorporated into the sample during the embryo biopsy for PGD, which could alter the final result of this technique.
How effective is ICSI with testicular biopsy?
It will depend on each case. If in the testicular biopsy at least one quality spermatozoon is obtained for each egg to be fertilized, the probability of success will be high. If, on the other hand, no live sperm are found in the biopsy, microinjection will not be possible.
How many tries with ICSI before getting pregnant?
While some achieve pregnancy on the first attempt, others need two, three or more attempts to finally become pregnant. Since a number of factors could have an impact on the outcome of ICSI, we cannot provide you with an specific figure.
Egg and sperm quality, embryo quality, the cause of infertility, and the conditions of the endometrial lining are some factors that could influence the success rate of ICSI.
Why is ICSI not used in all IVF procedures?
Infertility treatments always aim to imitate the natural process of conception as much as possible as the first option. With conventional IVF, the sperm reaches and penetrates the egg by itself. However, in IVF with ICSI procedures, the embryologists injects the sperm directly into the egg. This is the reason why conventional IVF is more similar to natural conception.
Also, the sperm is chosen by natural selection, while with ICSI it is done following the criterion of the specialist. A sperm capable of fertilizing the egg with their own power is a healthy one, and therefore one able to create viable embryos.
Recommended reading
A variant of ICSI is PICSI - physiological ISCI. To learn more about this technique and its uses please visit the following article: Physiological ICSI.
Alternatively, if you need more information about other assisted reproductive techniques, you can find it in this article: What are infertility treatments?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Reproducción Asistida ORG. Video: ¿Qué tipo de técnica FIV es la más empleada y por qué? (Which technique is the most widely used one and why?), by Miguel Dolz Arroyo, MD, PhD, Jun 16, 2014. [See original video in Spanish].
Aytoz A., Camus M., Tournaye H., Bonduelle M., Van Steirteghem A. and Devroey P. (1998): Outcome of pregnancies after intracytoplasmic sperm injection and the effect of sperm origin and quality on this outcome. Fertil. Steril. 70: 500-505.
Bourne H. Richings N. Harari O. Watkins W. Speirs A.L. Johnston W. I. H. Baker W.G. (1995). The use of intracytoplasmic sperm injection for the treatment of severe and extreme male infertility. Reprod Fertil Dev 7
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB (2006). A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update; 12:685-718.
Bruno I, Pérez F, Tur R, Ricciarelli E, De la Fuente A, Monzó A. et al. (2005). Grupo de interés en Salud Embrionaria. Sociedad Española de Fertilidad. Embarazos múltiples derivado de FIV-ICSI en España: Incidencia y criterios sobre la transferencia embrionaria. Rev Iberoam Fertil; 22 (2): 99-110.
ESHRE Capri Workshop Group. Intracytoplasmic sperm injection (ICSI) in 2006 (2007): evidence and evolution. Hum Reprod Update;13:515 – 526.
Esteves SC, Roque M, Bedoschi G, Haahr T, Humaidan P. Intracytoplasmic sperm injection for male infertility and consequences for offspring. Nat Rev Urol. 2018 Sep;15(9):535-562.
Fernández A, Castilla JA, Martínez L, Núñez AI, García-Peña ML, Mendoza JL, Blanco M, Maldonado V, Fontes J, Mendoza N (2002). Indicadores de calidad asistencial en un programa de FIV/ICSI. Rev Iberoam Fertil; 19: 249-52.
Jacob S., Drudy L., Conroy R. and Harrison R.E (1998): Outcome from consecutive in-vitro fertilization/ intracytoplasmic sperm injection attempts in the final group with urinary gonadotropins and the first group treated with recombinant follicle stimulating hormone. Hum. Reprod. 13: 1783-1787.
Johnson MD (1998). Genetic risks of intracytoplasmic sperm injection in the treatment of male infertility: recommendations for genetic counseling and screening. Fertil Steril; 70(3): 397-411.
Lanzerdorf S., Maloney M., Ackerman S., Acosta A., Hodgen G. (1988). Fertilizing potential of acrosome-defective sperm following microsurgical injection into eggs. Gamete Res
Markert Ch (1983). Fertilization of mammalian eggs by sperm injection. J Exp Zool228: 195-201.
Moomjy M, Sills ES, Rosenwaks Z, Palermo GD (1998). Implications of complete fertilization failure after intracytoplasmic sperm injection for subsequent fertilization and reproductive outcome. Hum Reprod; 13:2212 – 2216.
Palermo C.D. Cohen J. Rosenwaks Z (1996). Intracytoplasmic sperm injection: a powerful tool overcome fertilization failure. Fertil Steril 6: 899-908.
Palermo C.D., Joris H. Devroey P. Van Steirteghem A.C. (1992). Pregnancies after intracytoplasmic injection of single spermatozoa into an oocyte. Lancet, 340
Palermo C.D. Cohen J. Alikani M. Adler A. Rosenwaks Z. (1995). Development and implementation of intracytoplasmic sperm injection. Reprod Fertil Dev 7
Palermo GD, Neri QV, Rosenwaks Z. To ICSI or Not to ICSI. Semin Reprod Med. 2015 Mar;33(2):92-102.
P.J. Sánchez Abad; L.M. Pastor y M. Sánchez Abad. (1999). Situación actual de la inyección intracitoplasmática de espermatozoides (lCSI): Principales dilemas éticos. En: Cuadernos de Bioética 1999/1ª. Asociación Española de Bioética y Ética Médica (AEBI)
Rubino P, Viganò P, Luddi A, Piomboni P. The ICSI procedure from past to future: a systematic review of the more controversial aspects. Hum Reprod Update. 2016 Mar-Apr;22(2):194-227.
Sociedad Española de Fertilidad. Registro Nacional de Actividad 2022-Registro SEF. (Ver)
Teixeira DM, Hadyme Miyague A, Barbosa MA, Navarro PA, Raine-Fenning N, Nastri CO, Martins WP. Regular (ICSI) versus ultra-high magnification (IMSI) sperm selection for assisted reproduction. Cochrane Database Syst Rev. 2020 Feb 21;2(2):CD010167.
Zhao J, Yan Y, Huang X, Li Y. Do the children born after assisted reproductive technology have an increased risk of birth defects? A systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2020 Jan;33(2):322-333.
Zheng Z, Chen L, Yang T, Yu H, Wang H, Qin J. Multiple pregnancies achieved with IVF/ICSI and risk of specific congenital malformations: a meta-analysis of cohort studies. Reprod Biomed Online. 2018 Apr;36(4):472-482.
FAQs from users: 'In which cases is ICSI used automatically?', 'What are the advantages and disadvantages of ICSI over IVF?', 'What are the risks of ICSI treatment for the patient?', 'What are the pros and cons of ICSI over IVF?', 'What is the difference between ICSI and IUI?', 'When PGD/PGS is required, what is better, ICSI or IVF?', 'How effective is ICSI with testicular biopsy?', 'How many tries with ICSI before getting pregnant?' and 'Why is ICSI not used in all IVF procedures?'.
Authors and contributors


More information about Michelle Lorraine Embleton

















Hello. I’ve just went through my first ICSI. They managed to retrieve 26 eggs, of which 12 fertilised. Unfortunately only 2 developed with a potential 3rd(the next day was advised it didn’t make it). I’m 38. Apparently have no problems on my side. Can you advise on reasons why only 2 developed? I had them implanted both, but 2 days ago I started bleeding, so probably with no success.
Thank you.
Dear Alexandrina,
Sometimes, embryos may stop developing for a number of reasons, including the presence of chromosomal abnormalities. It’s common that not all embryos make it to day 5 for various reasons.
As for bleeding after embryo transfer, I don’t know when did you had the embryos transferred, but depending on the day, it may be implantation bleeding, which is a very good sign.
I hope this helps,
Best
Hi everyone,
my partner of 10 years and I have been trying for pregnancy. However, I’m still not pregnant after 2 years. We need a doctor to help us. Since we are newbies, we don’t know whom to contact or turn to.
Can someone help us here?
Hi Diane,
if you need assisted reproductive technologies in order to achieve a pregnancy and you need help in choosing a fertility center where to perform it, I recommend you access the Fertility Report. This is a completely free tool with which you will receive a personalized list of the clinics in your area of interest that meet our quality criteria and that best suit your needs.
In addition, you will get quotes, services included, and not included to avoid surprises.
I hope you find it useful.
Best regards