In recent years, the incidence of some form of cancer in women of reproductive age has increased.
Advances in medicine and oncology treatments have allowed these women to survive long enough. However, anti-cancer therapies have the downside of affecting fertility.
For this reason, it is important for women facing chemotherapy or radiotherapy to be informed about fertility preservation techniques, as this will give them the chance to become mothers once the cancer has been overcome.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 3.5.
- 3.6.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 4.6.
- 5.
- 6.
- 7.
Cancer and fertility in women
In recent years there has been an increase in the number of breast cancer cases in women aged 25-39 years. The second type of cancer with the highest incidence and prevalence in women is uterine cancer. In addition, it is estimated that about 25% of women who have had cancer have not been able to fulfill their reproductive desire.
The survival of young patients from breast, uterine and other cancers has been significantly increased by the combination of high-dose chemotherapy and radiotherapy. New advances in research have also contributed.
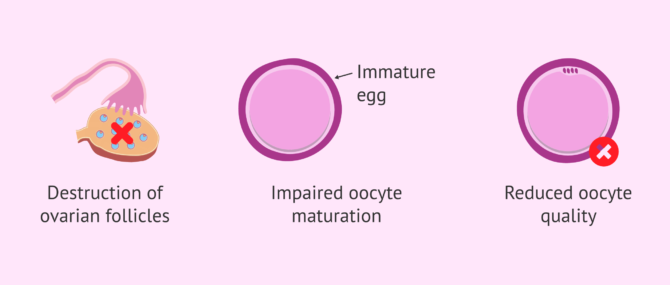
However, chemotherapy has effects on women's fertility such as the following:
- Destruction of ovarian follicles
- Alteration of the egg maturation process.
- Reduction in the quality of the eggs.
On the other hand, radiotherapy is capable of generating in women early ovarian insufficiency (IOP), destruction of immature eggs, etc. depending on where the ionizing radiation is received.
If you want to learn more about the effect of cancer on men's and women's fertility, you can read more following the following link: How does Cancer affect Fertility in Men and Women?
Alterations after cancer treatment
Once the oncological treatment is finished, diverse alterations in the feminine fertility can occur:
- Premature ovarian failure or transitory amenorrhea, i.e., temporary absence of menstruation.
- Recovery of menstrual cycles but not of fertility.
- Damage to the genetic material (DNA) of the eggs.
- Alterations in the fallopian tubes that would cause problems when getting pregnant.
It is really important that oncologists talk to the patient about the effects of oncological treatments on her reproductive capacity and explain the different options that exist to preserve her fertility.
Ideally, this conversation should take place before treatment begins, but there are also options for preserving fertility during chemotherapy or radiation therapy treatment.
Depending on the type of cancer, the age of the woman and the stage of the disease, the most appropriate option will be decided so that the woman can fulfill her desire to be a mother in the future.
Techniques before starting chemotherapy and radiation therapy
A woman diagnosed with cancer should be informed of the possible consequences of cancer treatments, as well as techniques for preserving her fertility before starting them.
Egg Vitrification
This method consists of freezing the mature eggs obtained after controlled ovarian induction through the vitrification technique (ultra-fast freezing), in which the eggs are passed from 15ºC to -196ºC. In this way, the oocytes are conserved unaltered for an infinite time, regardless of whether the woman is subsequently subjected to oncological treatment.
In the egg vitrification, due to the speed with which the change from one temperature to another takes place, there is no formation of ice crystals. That is why, the survival of the eggs is high and it is possible to delay motherhood with a good chance of success.
Once the woman has overcome the disease and is ready to become a mother, the eggs are devitrified and inseminated using an in vitro fertilization (IVF) technique. The embryos created are then transferred to the woman's uterus.
To act as soon as possible against cancer is crucial, but to perform egg vitrification it is necessary to delay the start of treatment by about 1 month. This postponement of cancer treatment is not always possible. Also, in the case of a hormone-dependent tumor, such as breast cancer, this option is not recommended because the tumor could increase in size.
Egg vitrification is also recommended for young single women who want to maintain their chances of becoming mothers in the future. In addition, it can be carried out on women who for personal or professional reasons wish to delay the time of having a child.
Embryos Cryopreservation
Embryo cryopreservation is another highly effective procedure for preserving female fertility. It consists of freezing the embryos generated prior to oncological treatment with the woman's oocytes and the sperm of her partner or an anonymous donor. It can be carried out by slow freezing or vitrification.
When this technique is carried out to preserve fertility, it is recommended to obtain embryos in the blastocyst state, that is, the embryo on day 5-6 of development and vitrify them.
The points to take into account in the cryopreservation of embryos are:
- A male partner or donor sperm is needed.
- The woman will undergo ovarian stimulation and puncture for egg retrieval.
- Carry out an IVF treatment to generate the embryos and allow them to evolve until day 5-6 to obtain them in a state of blastocyst. This takes a minimum time of 2 weeks.
It is very important that there is a fluid, rigorous and sincere communication on the part of the oncologist responsible for the treatment. In this way, decisions can be made more safely and coherently for each case.
If you are considering preserving your fertility to have a baby in the future, we recommend that you start by getting a Fertility Report. In 3 simple steps, it will show you a list of clinics that fit your preferences and meet our strict quality criteria. Moreover, you will receive a report via email with useful tips to visit a fertility clinic for the first time.
Surgery for ovarian cancer
Young women with cancer in one ovary have the option of removing this diseased ovary to preserve the other that is healthy.
It should be the oncologist who verifies that the removal can be performed without risk. To be able to perform this technique, the tumor must be:
- Slow-growing.
- With few possibilities of propagation.
- Low malignancy.
- Germ cell and borderline tumors.
A thorough follow-up is done to make sure that no tumor appears in the other ovary. With this option, the woman remains fertile and can achieve pregnancy naturally. The doctor will remove the damaged ovary and leave the healthy ovary and uterus in place.
If there is a risk that cancer will recur, the oncologist may remove the remaining ovary after the reproductive desire has been fulfilled.
Techniques during cancer treatment
Once a woman has undergone cancer treatment with chemotherapy and/or radiotherapy, the possibilities for preserving fertility are different. These are detailed below.
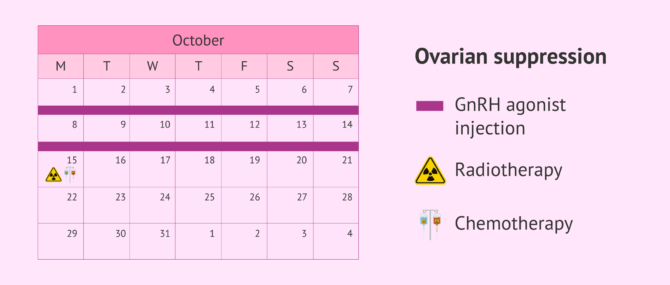
Ovarian suppression
This procedure causes the ovaries to stop working during chemotherapy and radiation therapy, protecting them from the harmful effects these treatments cause. The goal is to decrease the normal activity of the ovary by causing fewer damaged eggs. In addition, several studies indicate that this technique appears to work best in women younger than 35 years.
GnRH agonists (gonadotropin-releasing hormone) are injected two weeks before starting pelvic radiation therapy or chemotherapy. It is based on the use of hormonal medications that have prolonged action and that will cause a woman to go through menopause for a short time.
Ovarian suppression is an experimental procedure, i.e. a technique without proven efficacy and safety. Since more research is still needed, it is recommended to combine it with an egg or embryo vitrification technique.
Some drawbacks of this technique are the appearance of hot flashes, weakness, and the use of expensive medications.
Protection of the ovaries
Radiation therapy or total body irradiation can have an effect on the ovary, causing lesions that will lead to infertility or early ovarian failure. In addition, several studies have shown that women treated with radiation therapy to the abdominal area have an increased risk of miscarriage.
Therefore, the ovaries must be protected with an apron when there is a radiotherapy treatment in the pelvis or a nearby region. More studies are still needed to demonstrate its efficacy.
Ovarian tissue freezing
Ovarian tissue freezing is an experimental technique whose efficacy and safety has not been demonstrated. However, it is recommended for prepubertal girls with cancer.
It consists of removing all or part of the ovary by cutting the tissue from the ovarian cortex and cryopreserved using the vitrification technique. It is done by laparoscopy, which is minor surgery through a thin tube that is inserted through an incision made near the navel.
When a woman wishes to become a mother after cancer treatment and is fully prepared, the ovarian tissue is thawed and implanted near the fallopian tubes. This tissue is reactivated and produces eggs again, which can be collected and used in an IVF treatment.
Actually, this method is not recommended in women with cancers of the blood (such as leukemias or lymphomas) or ovarian cancer because of the risk of cancer cells in the implant.
The cost of this technique is very variable, as extraction, freezing, and transplantation must be performed.
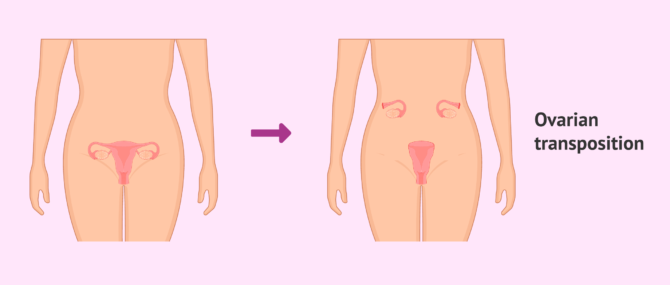
Ovarian transposition
The method of ovarian transposition, also known as ovariopexy, is carried out to prevent possible lesions in the gonad by ionizing radiation. It may only be used in cases of radiation to the pelvis and is permitted before and after puberty.
Ovariopexy is the removal of the ovaries from the radiation zone. To do this, the surgeon moves the ovaries to another part of the body, away from the place where radiation therapy is to be performed. Once performed, its effect can be tested by determining gonadotropin or steroid hormones.
This change in the ovaries should be done just before radiation therapy treatment begins to prevent the ovaries from coming back into place over time.
After the end of the radiotherapy treatment, the ovaries are returned to their original position. Approximately 50% of women have a natural return to menstruation.
Ovarian transposition is recommended for women under the age of 40 who do not show metastasis. It has also been demonstrated in women affected by Hodgkin's Lymphoma.
The complications that can occur after ovarian transposition are:
- Vascular lesions.
- Infarction of the fallopian tube by torsion of the same.
- Formation of cysts.
- Appearance of uterine adhesions.
In vitro oocyte maturation
The in vitro oocyte maturation preservation technique consists of an experimental technique applied through the extraction of eggs from the woman or from ovarian tissue. Prophase I oocytes, i.e. small immature oocytes, are obtained and matured in vitro in the laboratory.
This technique has no risk of ovarian hyperstimulation; however, it carries the risk of an increase in chromosomal, genetic, and epigenetic alterations.
Epigenetic alterations are changes in the chemical structure of DNA by the insertion or elimination of methyl groups in DNA that do not alter the coding sequence.
The characteristics of in vitro oocyte maturation are:
- There is no ovarian stimulation, so there is no risk of hyperstimulation.
- Reduction of the costs derived from ovarian stimulation.
- Less complexity.
- Lower implantation rate.
- Higher abortion rate.
If you would like to read more about this topic, we recommend you to visit the following article: In Vitro Maturation of Oocytes (IVM) in Assisted Reproduction.
Radical Cervectomy
This is an option for women with early cervical cancer. It consists of removing the cervix leaving the uterus and ovaries in place. This will connect the uterus to the upper part of the vagina through a band.
Women can achieve pregnancy after cervical ectopy; however, there is a risk of miscarriage and premature births.
FAQs from users
In which women is the preservation of ovarian tissue indicated?
The freezing of ovarian tissue is part of the fertility preservation techniques that are currently available for those women who, in the face of oncological or surgical treatments, may put their reproductive capacity at risk.
The procedure consists of the surgical extraction of the most superficial layer of one of the ovaries and the conservation in liquid nitrogen with cellular protective means. Once the oncological or surgical process is over, that fragment of ovary will be placed again in the place from which it was extracted.

At present, the speed of programming ovarian stimulation cycles to obtain oocytes for cryopreservation means that the preservation of ovarian tissue is relegated to those cases in which oncological/surgical treatment must be applied immediately, when the patients are girls who have not yet had their first menstruation or in those patients with pathologies in which ovarian stimulation to obtain oocytes is contraindicated.
Is there enough time left to freeze eggs before cancer treatment?
Cancer treatment may occasionally require removal of the ovaries or administration of chemotherapy or radiation therapy. This often results in a loss of fertility. However, in many situations, with adequate planning it will be possible to preserve the fertility of these patients so that they can become mothers in the future. The most important thing in this sense is to consult a fertility specialist as soon as the malignant pathology is diagnosed.
Read more
Is in vitro oocyte maturation available?
In vitro oocyte maturation is considered an experimental technique in the field of assisted reproduction to preserve fertility in women. This means that it consists of a technique whose efficacy and safety has not yet been demonstrated.
Are assisted reproduction techniques necessary after ovarian transposition?
Several assisted reproduction techniques may be necessary after ovarian transposition to preserve a woman's fertility.
It is possible that the ovaries are less accessible, which hinders the process of ovarian puncture to obtain eggs.
What are the techniques for preserving fertility in women with cancer with proven safety and efficiency?
The techniques to preserve fertility that are not considered experimental and have proven safety and efficacy are egg vitrification, embryo cryopreservation and ovariopexy or ovarian transposition.
How long should GnRH injection be given in the case of ovarian suppression?
The injection of GnRH for ovarian suppression must be repeated every month for the duration of the oncological treatment.
Recommended readings
If you want to know the methods of preserving fertility, you can read the article Fertility Preservation – Cost & Options for Retaining Your Fertility
In addition, if you want to learn about fertility problems, we recommend you to read the following link: Fertility problems
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Ana Cobo, Juan Antonio García-Velasco, José Remohí, Antonio Pellicer. Oocyte vitrification for fertility preservation for both medical and nonmedical reasons. Fertil Steril. 2021 May;115(5):1091-1101. doi: 10.1016/j.fertnstert.2021.02.006 (View)
Anna Marklund, Frida E Lundberg, Sandra Eloranta, Elham Hedayati, Karin Pettersson, Kenny A Rodriguez-Wallberg. Reproductive Outcomes After Breast Cancer in Women With vs Without Fertility Preservation. JAMA Oncol. 2021 Jan 1;7(1):86-91. doi: 10.1001/jamaoncol.2020.5957 (View)
Callejo J. Preservación de la fertilidad en la paciente oncológica. ED. Glosa 2009. The Practice Committes of the ASRM and teh SART. Madure oocyte criopreservation: a guideline. Fertil. Steril. 2012.
Fertility Assessment and treatment for people with fertility problems. NHS. NICE clinical guideline 156. February 2013
Findeklee S, Radosa JC, Takacs ZF, Hamza A, Sima RM, Solomayer EF, Sklavounos P. Fertility preservation in female cancer patients-state of the art. Minerva Ginecol. 2019 Apr 15. doi: 10.23736/S0026-4784.19.04387-9.
Gris, JM, Callejo, J. Técnicas de preservación de la fertilidad. Sociedad Española de Fertilidad (SEF).
Jacques Donnez, Marie-Madeleine Dolmans. Fertility preservation in men and women: Where are we in 2021? Are we rising to the challenge?Fertil Steril. 2021 May;115(5):1089-1090. doi: 10.1016/j.fertnstert.2021.03.028. Epub 2021 Apr 3 (View)
Melo AS, Paula CTV, Rufato MAF, Rufato MCAC, Rodrigues JK, Ferriani RA, Barreto J. Fertility optimization in women with cancer: from preservation to contraception.JBRA Assist Reprod. 2019 Apr 10. doi: 10.5935/1518-0557.20190011.
Pesce, R, Marconi, M, Vélez, C, Marconi, G, Glujovsky, D, Baronio, M, Coscia, A. Preservación de la fertilidad. Almer.Reproducción 2017;32:34-39.
Petra Vuković, Miro Kasum, Jelena Raguž, Nikolina Lonjak, Sara Bilić Knežević, Ivana Orešković, Lidija Beketić Orešković, Ermin Čehić. FERTILITY PRESERVATION IN YOUNG WOMEN WITH EARLY-STAGE BREAST CANCER. Acta Clin Croat. 2019 Mar;58(1):147-156. doi: 10.20471/acc.2019.58.01.19 (View)
FAQs from users: 'In which women is the preservation of ovarian tissue indicated?', 'Is there enough time left to freeze eggs before cancer treatment?', 'Is in vitro oocyte maturation available?', 'Are assisted reproduction techniques necessary after ovarian transposition?', 'What are the techniques for preserving fertility in women with cancer with proven safety and efficiency?' and 'How long should GnRH injection be given in the case of ovarian suppression?'.
Authors and contributors
More information about Cristina Algarra Goosman












Hello, I have been diagnosed with lung cancer. I have 1 child but in the future, my husband and I would like to have more. I have been recommended to vitrify eggs but I am wondering is it better to have eggs or embryos? Thank you
Hi Nora,
When faced with fertility preservation, it is recommended to cryopreserve embryos on eggs as these are more likely to vitrify with crystals since the egg is a water-filled cell. If there is a possibility I would recommend that you cryopreserve embryos, this will also ensure that the quality of the frozen embryos is genetically correct.
I hope I have helped you,
Best regards.
Hi,
My sister has been diagnosed with ovarian cancer, is it true that she can freeze her eggs in order to preserve her fertility?
Hello Jessy,
Yes, it is the best way to preserve fertility when cancer is diagnosed. Indeed, before the treatments, you cannot know what will be the damages. So, it is the best way!
Have a nice day!