In recent years, stress and anxiety have become one of the leading causes of sick leave in our society. Such is the importance that many scientists have tried to address the following question: Can anxiety be a cause of infertility?
What is certain is that scientific society is divided between studies that show that men and women with high levels of anxiety tend to ovulate less and have poorer semen quality; and studies that claim that the mechanism by which stress affects fertility has not yet been discovered. So there is one truth that is undeniable: there is still no scientific evidence that can prove that emotional stress influences fertility.
However, exposure to high levels of anxiety can lead to emotional overload. This can make a person feel depressed and unable to undergo assisted reproduction treatment, abandoning the project of having a child.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 3.2.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 5.6.
- 6.
- 7.
- 8.
What is stress?
Stress is a reaction of the body produced by tension or a situation that causes uneasiness. If this anxiety lasts over time, it can cause psychosomatic and physical disorders that can alter health.
However, despite being the cause of various diseases today, stress is a survival mechanism that has been preserved over time. It is the process by which animals and humans have survived throughout evolution, preparing them to flee or fight a dangerous situation and save their lives.
Nowadays, the unbridled lifestyle of the population has put the stress mechanism in the spotlight, going from being an ally to surviving danger to the new disease of the 21st century.
This is due to the fact that the stimuli that produce anxiety do not disappear, because the body feels constantly in danger, and the alert mechanisms remain continuously on.
How does stress act on our body?
When there is a situation that produces anxiety, the whole body is put on alert and produces a reaction, both physical and hormonal, that prepares to react to that moment of anxiety. The brain picks up signals that are perceived as threatening and the most primary part of the brain is activated, leaving reasoning aside.
The body begins to secrete large amounts of hormones such as adrenaline and cortisol, which will cause the body to react to danger:
- Adrenaline: it is responsible for administering emergency energy to those parts of the body that will need it to flee or fight. Thus, adrenaline causes blood pressure and heart rate to increase to keep the individual active and alert.
- Cortisol: also called the stress hormone, it is secreted only if the fear is persistent over time. The role of cortisol focuses on maintaining vital signs and suppressing functions that are not necessary for survival. To do this, this hormone will cut off the energy supply to the rest of the organs that do not need it and divert it to the muscles and the brain.
The physiological process that can save our lives in times of risk is also a cause of illness if anxiety levels are not reduced. If stress becomes chronic, the hormones cease to have an effect and pass into the bloodstream, where they can accumulate in large quantities and have a harmful impact on the body.
Stress infertility
Unlike in humans, animal studies have already linked the mechanisms by which chronic stress affects fertility. However, although these processes have not been understood in humans, it is known that their origin lies in the high concentrations of corticosteroids in the blood and their interactions with other hormones, including sex hormones.
Chronic stress affects both female and male fertility by interfering with menstrual cycle control and sperm formation, respectively. We discuss this in the following sections.
Female sex hormones disrupted by chronic stress
Under normal conditions, FSH and LH are responsible for the growth and release of eggs in women, while estrogens and progesterone regulate the menstrual cycle and prepare the endometrium to receive the embryo.
Continuous anxiety can influence the hormonal control that takes place in the brain. This is because increased concentrations of the stress hormone cortisol can alter the frequency of GnRH (FSH and LH gonadotropin-releasing hormone) release:
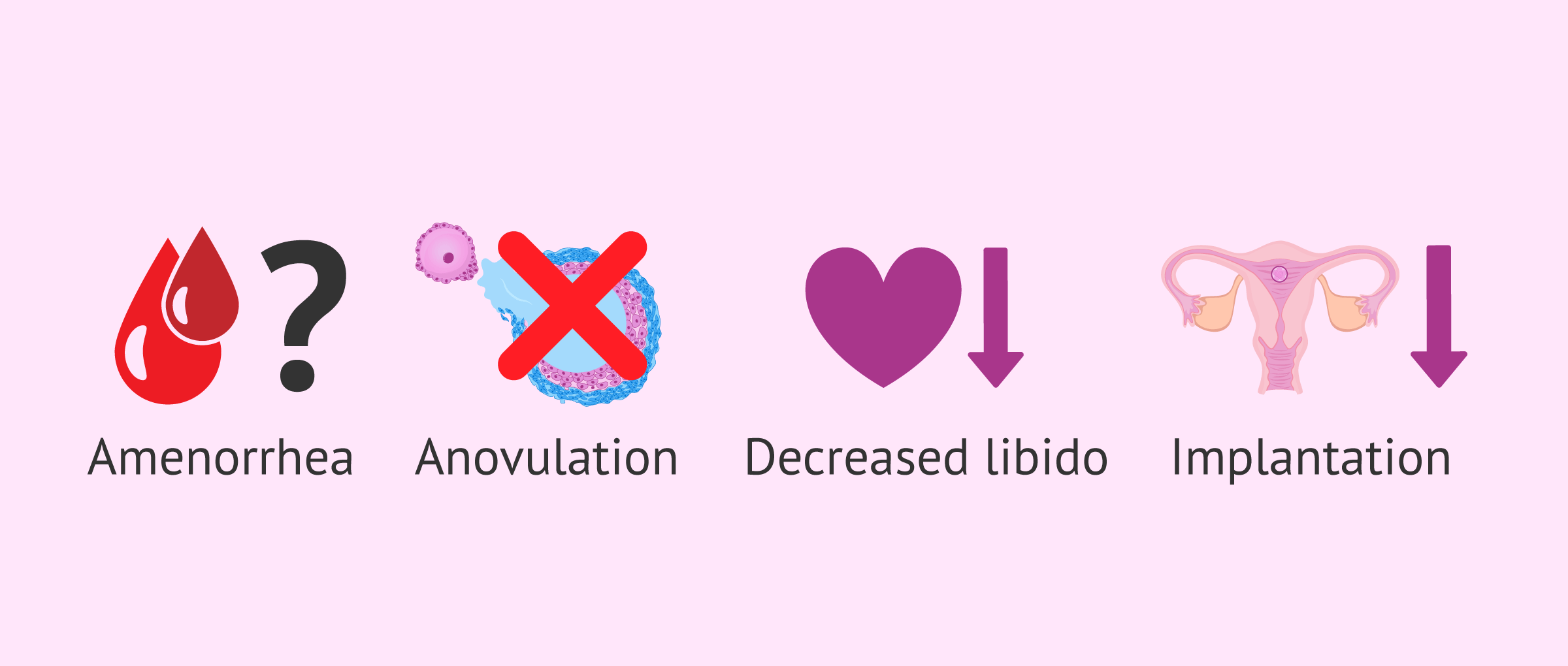
- Decreased secretion of GnRH pulses can lead to amenorrhea (absence of menstruation)
- Increased frequency and overexposure of GnRH leads to anaovulation (absence of egg release from the ovary)
Increased cortisol may also ultimately influence estrogen and progesterone concentrations:
- The follicles do not receive enough hormone to grow and mature properly.
- Decreased libido and sexual frequency, so the chances of achieving pregnancy decrease if the sexual frequency is reduced.
- In the case of fertilization, the implantation of the embryo in the uterus depends on good estrogen and progesterone hormone levels.
Male sex hormones disrupted by chronic stress
Under normal conditions, FSH and LH act by regulating the secretion of testosterone in the testis. Testosterone is the hormone that ultimately intervenes and promotes spermatogenesis, that is, the creation of spermatozoa.
When elevated levels of cortisol are present in the blood, due to constant fear, the concentrations of hormones regulated by the brain are altered. This increases FSH and LH levels and reduces testosterone production, altering sperm production.
This hormonal alteration has a negative impact on sperm parameters, reducing the concentration, motility, and morphology of the samples because the spermatogenesis process is altered.
Infertility studies have not only detected a decrease in the quality of seminal samples in men affected by chronic stress, a decrease in ejaculate volume, a decrease in libido and erectile dysfunction problems can also be observed. As a consequence, there may be a decrease in sexual activity and therefore less likelihood of pregnancy.
In the article Can stress cause infertility? you can continue reading about the effects of stress on male fertility.
Anxiety in assisted reproductive treatments
As we have said from the beginning of this article, despite the different scientific studies that have tried to link stress as a cause of infertility, this relationship has not yet been proven. However, it is clear that infertility and assisted reproduction treatments cause a great emotional burden.
Delayed childbearing or social pressure can cause many couples to have anxiety, depression, or guilt about not achieving the desired pregnancy. In addition, if such patients decide to undergo assisted reproduction treatment, stress levels skyrocket. It is therefore very common for couples undergoing fertility treatment to encounter a very high level of psychological exhaustion and suffering.
This is why, for years now, infertility clinics have not only been trying to deal with fertility problems medically but are increasingly developing departments focused on the patient's well-being.
Those patients who need it will be supported by expert professionals in psychology. This measure is essential to alleviate the psychological burden of these patients and to ensure that they do not abandon their reproductive treatments due to emotional exhaustion.
As we have seen, it is highly disproven that those infertile couples who decide to face a fertility process have high levels of anxiety and fear. If you are interested in continuing to read about the emotional burden faced by those who decide to undergo IVF treatment, you can read more in the article Stress and assisted reproduction.
FAQs from users
Can nerves during the Two Week Wait affect the success of IVF?
Serious studies have measured the concentration of corticosteroids, the so-called stress hormone, in the saliva of women underdoing fertility treatments that suggest that stress directly affects the probability of pregnancy.
However, I must remember that the treatment, and even more, the so-called Two Week Wait period is really stressful for each and every woman, so the possible effect of stress on the success of the treatment has already been disclaimed.
In brief, it does affect stress in treatment, but this effect has already been calculated by the doctor when in consultation, you talked about the probability of treatment success.
Can suffering stress after embryo transfer affect the embryo?
There is controversy about the effect of stress on the results of assisted reproduction techniques, with studies showing a negative effect and others showing no association. In any case, the negative effects could be linked to the activation of the cortisol pathway and it is not known specifically which factors could influence it directly or indirectly (oocyte or implantation). There is no evidence of a direct effect at embryonic level.
What habits would you recommend to women who are currently on fertility treatment?
All in all, a healthy lifestyle, as well as trying to manage the stress and anxiety that many times arise when one is going through fertility treatment. Before getting started, and not only when they are carrying it out, I would recommend that they reduce the consumption of tobacco or quit smoking. Also, avoiding unhealthy habits is crucial, too. Preventing obesity and low weight, and avoiding street drugs and alcohol are basic tips as well.
Can having an anxiety attack during the two-week wait affect implantation?
No. According to a study carried out in Holland, anxiety levels prior to and during fertility treatment are not predictors of successful fertilization.
Therefore, suffering a panic attack during the twoo-week wait (understanding panic attack as the most intense manifestation of anxiety), does not interfere with embryo implantation. Anxiety in itself alters the emotional state of people, but it does not prevent an optimal result of the medical treatment.
It is of vital importance to attend to the psychological symptomatology that women have throughout the assisted reproduction treatments, since an emotional imbalance causes intense discomfort, even though it does not alter or modify the result of the same.
Is it possible that my anxiety is the cause of my infertility?
It is difficult to state that a patient's stress is the main cause of infertility. Many factors that may be involved in infertility must be taken into account.
However, many studies have shown that women and men with chronic stress had more alterations in the menstrual cycle and sperm quality.
Can stress cause azoospermia?
Yes, situations that increase anxiety or stress levels can alter the hormones that regulate sperm production, causing zero sperm count. However, these are situations of temporary azoospermia that allow the affected man to recover fertility after returning to normality. In other words, as soon as increased stress levels decrease and the man is more relaxed, sperm production starts anew and azoospermia disappears.
Recommended readings
The current lifestyle is responsible for multiple diseases suffered by the population today. The type of diet, pollution, and sedentary life is behind many of these problems, including infertility. That is why we address this topic in the article Influence of lifestyle on fertility and assisted reproduction.
Diet and obesity is a factor to be taken into account to take care of our health. Having an obesity problem has a great impact on our bodies and predisposes us to numerous health problems. A high BMI (body mass index) increases the chances of being infertile and causes a large number of problems when undergoing assisted reproduction treatment. If you are interested in this topic, do not miss the article Infertility due to alterations in BMI: underweight and obesity.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Macrae, C.N., Alnwick, K.A., Milne, A.B., and Schloerscheidt, A.M. (2002). Person perception across the menstrual cycle: Hormonal influences on social-cognitive functioning. Psychological Science, 13, 532–536.
Penton-Voak, I.S., Perrett, D.I., Castles, D.L., Kobayashi, T., Burt, D.M., Murray, L.K., and Minamisawa, R. (1999). Menstrual cycle alters face preference. Nature, 399, 741-742.
Vollman R F 1956 The Degree of Variability of the Length of the Menstrual Cycle in Correlation with Age of Woman Gynaecologia 142 (5): 310–314.
Chiazze L Jr Brayer F T Macisco J J Jr Parker M P Duffy B J 1968 The Length and Variability of the Human Menstrual Cycle JAMA, 203 (6) pp 377-380.
Fluhmann C F 1934 The Length of the human menstrual cycle. Department of obstetrics and gynecology American Journal of Obstetrics and Gynecology, 2 (1) pp 73-78.
Kelly-Weeder S., Cox CL. The impact of lifestyle risk factors on female infertility. Women Health. 2006;44(4):1-23.
Sołtysiak E. The influence of socioeconomic factors on female fertility. Ginekol Pol. 2005;76(12):986-90.
Sofikitis N, Migayana I, Dimitriadis D 1995 Effects of smoking on testicular function, semen quality and sperm fertilizing capacity. Journal of Urology 154, 1030–1034.
Hall L, Frayne J. Non-functional fertility genes in humans: contributory factors in reduced male fertility? Hum Fertil (Camb). 1999;2(1):36–41.
FAQs from users: 'Can nerves during the Two Week Wait affect the success of IVF?', 'Can suffering stress after embryo transfer affect the embryo?', 'What habits would you recommend to women who are currently on fertility treatment?', 'Can having an anxiety attack during the two-week wait affect implantation?', 'Is it possible that my anxiety is the cause of my infertility?' and 'Can stress cause azoospermia?'.
Authors and contributors


More information about Cristina Algarra Goosman









Hi, I have been going through several rounds of assisted reproduction treatments, I am not able to get pregnant, everyone tells me that when I relax I will get it, I am starting to think that this is the case, what can I do?
Hello Hasley,
Getting pregnant or not getting pregnant is not completely tied to your emotional state. It is true that it may play a role in favoring or facilitating pregnancy, but your stress levels are not consistent with achieving your pregnancy.
I recommend that you talk to your doctor who specializes in assisted reproduction to explain the reason or reasons why you are finding it somewhat difficult to get pregnant.
I understand that it is a tough process and you have to try to manage your emotions and rely on your inner circle.
I hope I have helped you.
Best regards.
Hi, I have a very stressful job and I’m afraid it might affect my baby, I’m 12 weeks pregnant and I haven’t mentioned it at work yet. What can I do?
Hello Leah,
External stress can have a negative impact on both you and your baby, therefore, trying to mitigate the controllable stress in your life would be ideal.
I encourage you to talk to your employer so you can both find a solution to decrease the levels of stress you experience at your job.
I hope I have helped.
Best regards