Testicular cancer is a rare pathology, but it mainly affects young men of childbearing age. Despite this, these tumors are curable in most cases and have a high survival rate.
Experts recommend early self-palpation of the testicles to detect any signs, such as a lump.
If testicular cancer is confirmed, all of these men are advised to freeze their semen prior to anti-cancer treatment in order to preserve their fertility.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 3.
- 4.
- 5.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 6.5.
- 6.6.
- 7.
- 8.
- 9.
Types of Testicular Cancer
Testicular cancer is the most common tumor in men between the ages of 15 and 40.
Although its mortality rate has dropped, the fact that it affects men of reproductive age makes testicular cancer very serious for couples who wish to have children.
Testicular cancer and especially the treatments to eradicate it (chemotherapy and radiotherapy) seriously affect male fertility.
The prognosis and treatment of testicular cancer basically depends on the type of tumor.
More than 90% of testicular tumors are generated in germ cells, where spermatogenesis or sperm production takes place. For this reason, these tumors are also called germ cell tumors which in turn differ in the following types:
Seminoma
Seminomas account for about 40% of testicular tumors. They are characterized as slow-growing tumors and do not usually spread to other parts of the body.
One tumor marker of this type of cancer is the hormone human chorionic gonadotropin(hCG), which is often elevated and used to diagnose testicular cancer.
In addition, seminomas are classified into two subtypes:
- Classical Seminoma
- it is the most common and usually affects men between the ages of 25 and 45.
- Spermatocytic Seminoma
- it is very rare and occurs at older ages, around age 65.
Since they are tumors that grow very slowly, their prognosis is very good and they are very sensitive to radiation therapy.
Non-seminoma
Non-seminoma tumors account for 60% of testicular tumors and tend to appear at younger ages, between 15 and 35 years. These tumors develop more quickly and are therefore more severe.
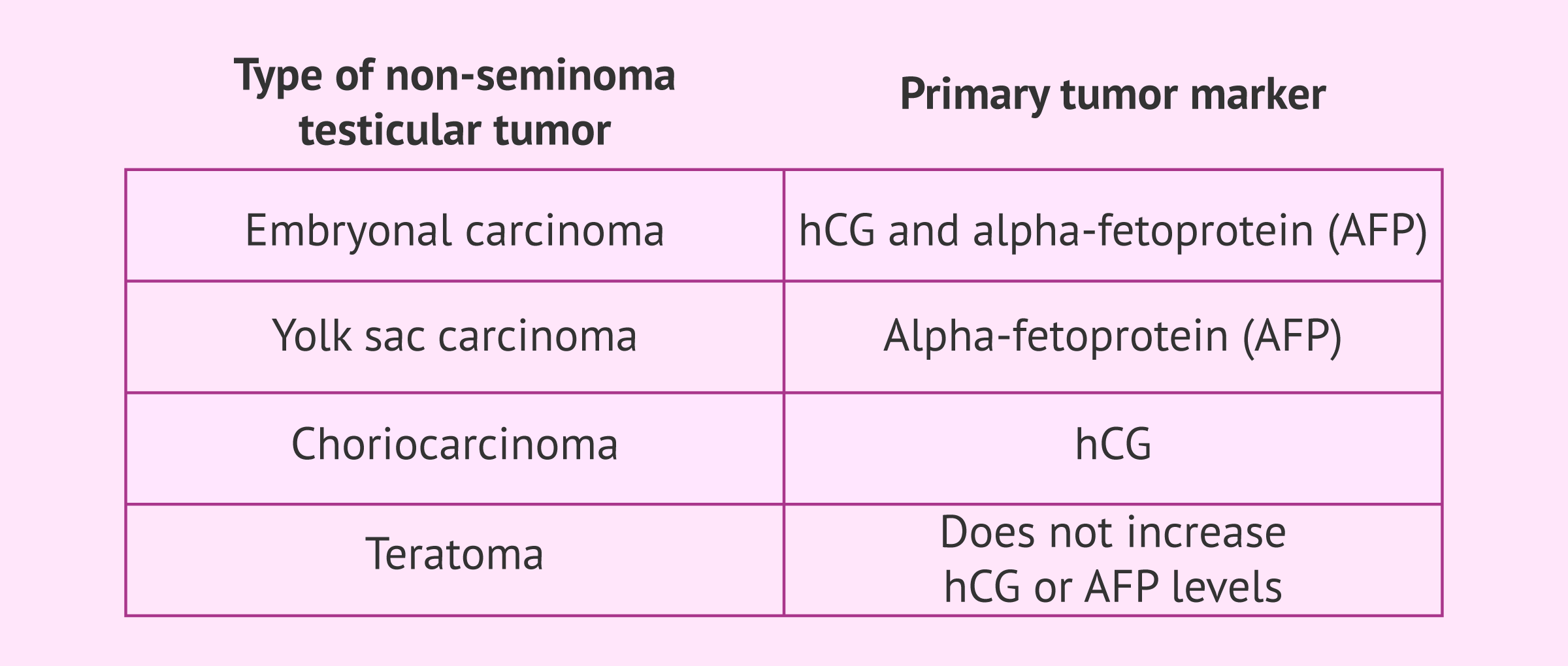
The main subtypes of non-seminoma germline tumors are as follows:
- Embryonal carcinoma
- it is the most frequent and very aggressive, as the tumor usually spreads to other organs quickly. The tumor markers for this type of cancer are hCG and alpha-fetoprotein (AFP).
- Yolk sac carcinoma
- it is the most common form in children and young people, and has great healing potential. However, at older ages they tend to be more complicated. The main tumor marker is also alpha-fetoprotein.
- Choriocarcinoma
- it is a very rare tumor affecting adult males. It grows very quickly and can spread to other parts of the body. The main tumor marker is hCG.
- Teratoma
- they are tumors that present cells of the three embryonic layers: the endoderm, the mesoderm and the ectoderm. They often appear as parts of mixed germ cell tumors and do not increase hCG or AFP levels.
Mixed germ cell tumors contain both seminoma and non-seminoma cells. This type of testicular cancer is treated in the same way as non-seminomas because they grow and spread like these.
What are the risk factors?
The exact causes of cancer are unknown, although it is known that an individual's lifestyle may be related and increase the likelihood of developing some type of tumor.
In particular, the risk factors for testicular cancer are as follows:
- Cryptorchidism: undescended testicle after birth.
- Family history of testicular cancer
- HIV infection.
- Environmental factors: men who are exposed to chemicals or radiation through their work.
- Genetic alterations such as Klinefelter Syndrome that cause abnormal development of the testicles.
- Race or ethnicity: White men have a higher incidence of testicular cancer than African-American men.
It should be noted that having one or more risk factors does not mean that a man will develop testicular cancer.
Symptoms and diagnosis of testicular cancer
First, all specialists in this field insist on the importance of making an early diagnosis of testicular cancer so that easy and quick treatment can be applied to remove the tumor without seriously affecting the health of the male.
To this end, it is recommended that all young people, from school age onwards, frequently perform testicular self-palpation in order to detect any sign of cancer, such as the appearance of a lump in the testicular area.
Other signs and symptoms to watch for in detecting testicular cancer include the following:
- Painless swelling or lump in the testicle
- Change in size, shape, and/or texture of the testicle
- Sensation of heaviness in the scrotum
- Usual symptoms by the testicular area
- Pain in the lower abdomen, back, or groin
- Fluid buildup in the scrotum
- Breast enlargement or sensitivity
Despite all of the above, some men have no symptoms of testicular cancer, and testicular cancer can only be detected by medical testing for other diseases. For example, by performing a testicular ultrasound during a male infertility study.
You can get all the detailed information on what diagnosis and self-examination should be to detect this type of tumor in the following article: Self Examination as a Preventive Measure against Testicle Cancer
Is there a treatment?
Treatment for testicular cancer will depend mainly on the type of tumor, its stage, and whether it affects one or both testicles.
The following is a description of the most important anti-cancer treatments:
- Surgery
- testicular removal (radical inguinal orchiectomy) is indicated for all types and stages of testicular cancer. Its cure rate is very high, although sometimes it is necessary to combine surgery with chemotherapy or radiotherapy to prevent relapses.
- Radiotherapy
- it is very effective in seminoma type tumors. High-powered energy rays are directed at the testicular area, destroying cancer cells. Its cure rate is over 95% in the early stages, but it is not very sensitive to non-seminoma tumors.
- Chemotherapy
- it is the treatment of choice when the tumor has spread to other parts of the body. It consists of administering drugs (bleomycin, carboplatin, etoposide or cisplatin, among others) to kill cancer cells.
In any case, the best therapeutic option will be determined by the specialist who knows the patient's situation perfectly. In addition, it is important to take into account the type and stage of cancer, as well as the patient's preferences.
Effects of testicular cancer on fertility
Testicular cancer does not cause male sterility problems. However, it is cancer treatments that cause many boys to have difficulty having children after they are cured.
The effects on male fertility will depend on the type of treatment. First, removal of a testicle does not alter male sexual function or seminal parameters. The remaining testicle is able to continue to produce the same amount of sperm and sex hormones to meet all needs.
On the other hand, radiotherapy and chemotherapy do affect the spermatogenesis of both testicles and may cause temporary or permanent infertility depending on the aggressiveness of the treatment.
For this reason, the best way to become a parent in the future is to preserve fertility by freezing semen. It is only necessary for the man to leave a semen sample in the laboratory after 3-5 days of abstinence.
You can get all the information about this procedure at the following link: What Is the Process of Freezing Sperm?
Do you need donor sperm for your fertility treatment cycle? Then we recommend that you get your Fertility Report now to find the most suitable clinic for you. Our thorough selection criteria when it comes to recommending clinics plus your particular needs equal the best fertility center for you. You will receive in your inbox a detailed report with the clinics that we recommend for your particular treatment, as well as the conditions that they offer for each program.
FAQs from users
Is it possible to have children with testicular cancer?
Yes, in order to carry out this treatment, an adequate semen sample will be taken prior to the oncological treatment in order to cryopreserve it.
If the oncological treatment has already been performed previously, we would have to evaluate its repercussion on spermatogenesis and decide the steps to follow according to the patient's history or case.
Is male fertility affected in men with only one testicle?
Possessing a single testicle, either from birth or due to a later occurence such as cancer, does not imply that there is a fertility problem. If the remaining testicle works correctly and the spermatogenesis is not affected, the man will be able to father a natural pregnancy without any problem.
What are the symptoms of advanced testicular cancer?
The symptoms of testicular cancer are not always easy to detect, either in early stages or in more advanced stages when the cancer has spread to other parts of the body.
However, some symptoms of this metastasis may be the following:
- Lower back pain if spread to lymph nodes.
- Difficulty breathing, coughing, or chest pain in case of pulmonary metastasis.
- Abdominal pain if there are metastases in the liver.
- Headache or confusion when the cancer spreads to the brain.
Can I have a relapse of testicular cancer?
Unfortunately, yes. People who have already suffered from testicular cancer are more likely to have this type of tumor again, for example in the other testicle. This is known as recurrent testicular cancer.
For this reason, it is very important that all patients who have had testicular cancer have regular check-ups with the urologist, especially the two years after the cancer therapy has ended.
Once the cancer has been overcome and the quality of the semen is low, would conventional IVF be recommended or would it be passed directly to an ICSI?
Once cancer has been treated, the male may be fertile. If this is not the case, he may resort to using the sperm he had frozen before his treatment. In these cases, since the semen is very valuable because of its scarcity (only one or two frozen samples), ICSI is used directly, since gestation can be achieved with a single spermatozoon. Thus, if more children were desired, there would still be a frozen sample.
Are there secondary testicular cancers?
Secondary testicular cancer is cancer that begins in an organ other than the testicle, but ends up spreading to the testicle. For this reason, this type of cancer is not known as testicular cancer, but receives the name of where it originated, even though it later spreads to the testicles.
Among the most common is testicular lymphoma, especially in men over 50 years of age. Other types of secondary testicular cancer are usually prostate, lung or kidney cancer, among others.
Recommended readings
If you are interested in learning more about the effects of cancer on male and female fertility, we recommend reading on: How Does Cancer Affect Male and Female Fertility?
On the other hand, we encourage you to learn more about preserving fertility in the next post: Fertility Preservation – Cost & Options for Retaining Your Fertility.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Aberger M, Wilson B, Holzbeierlein JM, Griebling TL, Nangia AK. Testicular self-examination and testicular cancer: a cost-utility analysis. Cancer Med. 2014 Dec;3(6):1629-34.
American Cancer Society. Cancer Facts & Figures 2017. Atlanta, Ga: American Cancer Society; 2017
Goriely A, Hansen RMS, Taylor IB, Olesen IA, Jacobsen GK, McGowan SJ, Pfeifer SP, McVean GAT, Rajpert-De Meyts E and Wilkie AOM. Activating mutations in FGFR3 and HRAS reveal a shared genetic origin for congenital disorders and testicular tumors. Nature Genetics 2009; 41:1247–1252
Horwich A, Shipley J, Huddart R. Testicular germ-cell cancer. Lancet. 2006;367:754-765
Moirano G, Zugna D, Grasso C, Mirabelli D, Lista P, Ciuffreda L, Segnan N, Merletti F, Richiardi L. Postnatal risk factors for testicular cancer: The EPSAM case-control study. Int J Cancer. 2017 Nov 1;141(9):1803-1810.
Ostrowski KA, Walsh TJ. Infertility with Testicular Cancer. Urol Clin North Am. 2015 Aug;42(3):409-20.
Viatori M. Testicular cancer. Semin Oncol Nurs. 2012 Aug;28(3):180-9.
FAQs from users: 'Is it possible to have children with testicular cancer?', 'Is male fertility affected in men with only one testicle?', 'What are the symptoms of advanced testicular cancer?', 'Can I have a relapse of testicular cancer?', 'Once the cancer has been overcome and the quality of the semen is low, would conventional IVF be recommended or would it be passed directly to an ICSI?' and 'Are there secondary testicular cancers?'.
Authors and contributors


More information about Cristina Algarra Goosman







Hello, I had some swelling in my scrotum and I was told that it is a hematocele. It is not clear to me what the treatment is and I would like to know if it could be cancer.
Hello Oscar,
The testicles are inside the scrotum and immersed in a small amount of fluid, hydrocele occurs when this fluid increases, it can be given by various causes such as surgery or trauma…
To treat it will depend on the complexity of the case, simple hydrocele usually disappears without treatment but if it is something more complex an intervention can be performed to remove the fluid from the scrotum or a scrotal aspiration.
I recommend you read the following article: What is a hydrocele?
I hope I have helped you,
A greeting
Hello, in the last few days I have noticed a kind of lump in my left testicle. I notice that it is somewhat swollen and kind of warm. Is that cancer?
Hi Skylar,
The symptoms you present may indicate the presence of a scrotal mass, these can be fluid accumulations or abnormal swollen or hardened growths.
To determine if the mass is benign or not it is important to see a doctor so that he/she can perform an examination and diagnosis of the scrotal mass. If he/she determines that there is a problem, he/she will proceed to recommend treatment.
I hope all goes well,
Best regards