Hysterosalpingography (HSG) is a study of the female reproductive tract in which the structure of the uterus and fallopian tubes is visualized in order to detect possible causes of infertility.
Although the most commonly used technique for this test is conventional HSG, which obtains images thanks to X-ray fluoroscopy, there are other newer types of HSG, such as hysterosalpingosonography (HSSG), which obtains images through sound waves, or virtual HSG.
Regardless of the technique used, hysterosalpingography is of great importance when diagnosing infertility and, therefore, all women who need to resort to assisted reproduction to become mothers should inform themselves about it.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 3.
- 3.1.
- 3.2.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 6.
- 7.
- 8.
Female fertility study
When a couple has been having unprotected sex for more than a year and still cannot get pregnant, both the man and the woman should undergo the necessary tests to help them find out the cause of infertility.
This period of attempts to achieve a natural pregnancy is reduced to 6 months if the woman is over 36 years old.
The most common fertility tests include a hormone analysis and ultrasound for the female, and a semen analysis for the male. With the first results obtained, the specialists can already get an idea of whether infertility has a female, male or combined cause.
In addition, based on these results, the woman will most likely be prescribed an additional test: hysterosalpingography. The importance of the latter in assisted reproduction is due to the following two reasons:
Conventional hysterosalpingography (HSG)
Classical or conventional hysterosalpingography is the best known since it is the usual technique for studying the patency of the fallopian tubes.
This study consists of introducing a radiopaque contrast liquid through the woman's cervix with the help of a catheter. The contrast liquid diffuses through the interior of the uterus and fallopian tubes until it is expelled into the peritoneal cavity.
Images of the organs through which the contrast flows are taken by X-ray, through a machine that is placed on the woman's abdomen.
If there is any alteration in the interior of the uterus or tubal obstruction that prevents the passage of contrast, these structures will not be seen in the images obtained and it can be concluded that the tubes are blocked.
If you want to obtain more detailed information about the whole process, we recommend you to access the following post: What is hysterosalpingography?
What are the advantages of HSG?
The benefits of conventional hysterosalpingography are as follows:
- It provides a lot of valuable information in a short time, lasting only 20-30 minutes.
- It can unblock the tubes during the passage of contrast and allow the woman to become pregnant easily.
- After the test, no radiation remains in the woman's body.
- There are no side effects from the use of x-rays in this examination.
Although hysterosalpingography requires X-rays, there are no side effects.
Risks
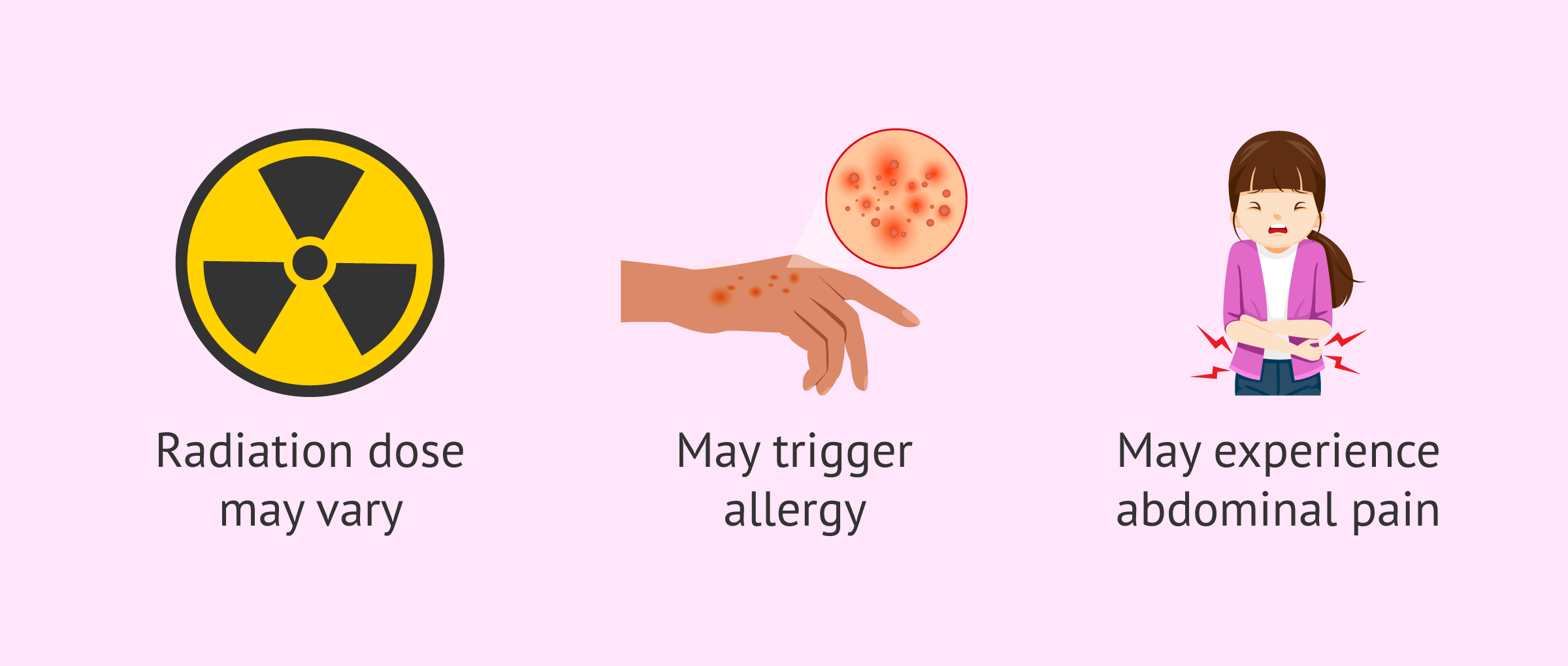
Although it is a safe technique, there are also some drawbacks and risks associated with classical hysterosalpingography:
- The effective radiation dose may vary in this procedure.
- Exposure to radiation is always associated with a slight chance of cancer, although this is a minimal risk.
- It can have serious consequences if you have a chronic inflammatory disease, pelvic infection, or sexually transmitted disease at the time of the test. Therefore, it is necessary to inform the physician beforehand.
- The ionized contrast used may trigger allergy in some patients.
- The woman may feel pain with the introduction of the liquid contrast or abdominal discomfort after the test is performed.
Hysterosalpingosonography (HSSG)
Hysterosalpingosonography or sonohysterosalpingosonography is a novel technique to diagnose alterations inside the uterus and fallopian tubes.
Unlike conventional HSG, HSSG uses sound waves to produce images of the reproductive organs through transvaginal ultrasound.
For this, a catheter is introduced through the vagina and a saline solution or foaming gel is injected, which will perform the same function as the radiopaque contrast medium, i.e., it will fill the uterus and tubes so that their interior can be visualized.
Depending on the liquid medium used in HSSG, there are two more specific types:
- HyCoSy
- from the abbreviation of Hysterosalpingo-Contrast-Sonography. This HSG model uses saline or a galactose solution to introduce them through the cervix.
- HyFoSy
- from the abbreviation of Hysterosalpingo-Foam-Sonography. This technique uses a foam that will expand through the uterus and tubes once introduced through the cervix.
In both cases, there are more advantages than using the classic HSG and, therefore, more and more women and gynecologists are in favor of using this new method.
Advantages
The following are the benefits of hysterosalpingosonography:
- It is a non-invasive technique and does not use X-rays.
- The discomfort caused is minimal and the woman does not usually feel pain after the test.
- It is a much faster technique, usually lasting about 10 minutes.
- It can be done at the gynecologist's office and the results can be obtained at the same time.
- The risk of allergy to the saline solution or foaming gel is minimal.
- The images obtained are sharper and of higher quality.
- No side effects have been reported for this technique.
Limitations
As in conventional HSG, HSSG cannot be performed in patients suffering from any sexually transmitted disease or pelvic infection.
Nevertheless, both HSG and HSSG provide information about the interior of the organs. To detect abnormalities of the uterine walls, ovaries or other structures of the pelvis, magnetic resonance imaging (MRI) would be necessary.
Virtual hysterosalpingography
Virtual hysterosalpingography (V-HSG) is another type of test to analyze the female reproductive system in a very complete way since it uses computed tomography (CT) to obtain images with much more anatomical detail.
The virtual HSG makes it possible to observe all the pelvic organs completely, both inside and on the walls. In addition, this technique offers the possibility of creating three-dimensional and endoscopic images, the final result being much more precise.
As in traditional HSG, iodinated contrast is also used to visualize the anatomical structures, but in this case the discomfort is less because it is not necessary to hold or traction the cervix for its introduction. Likewise, the radiation used for the analysis is also lower.
FAQs from users
What are the benefits of virtual hysterosalpingography?
Virtual hysterosalpingography would be the evolved version of this classic technique. The procedure is the same, but instead of performing a simple x-ray after the contrast injection, a computerized tomography (CT) scan is performed.
This technique allows us to have a better visualization of the uterus and the tubes since the CT scan offers much better image resolution. In addition, this test gives the possibility of observing the relationship of these organs with their neighbors, allowing 3D reconstruction of the images.
Even so, virtual hysterosalpingography is not routinely used in daily clinical practice, since the useful information it provides is not much greater than that of classic hysterosalpingography and the costs are much higher.
What are the differences between hysterosalpingography and hysterosonosalpingography?
Both Hysterosalpingography (HSG) and Hysterosonosalpingography (SHSG) are outpatient procedures used to evaluate tubal patency or obstruction in patients with infertility, as well as endocavitary uterine pathology.
HSG involves viewing the passage of an iodinated contrast dye through the uterus and tubes using several pelvic radiographs, while SHSG involves monitoring the passage of a gel-foam using pelvic ultrasound. Both are well tolerated, although referred pain is less with SHSG.
SHSG also has the advantage of avoiding the use of ionizing radiation and the risk of allergies to iodine, since a gel-foam composed of hydroxypropylcellulose and glycerol is used, and allergic reactions to it are rare. Compared to HSG, SHSG also allows concomitant visualization of the ovaries and myometrium.
In recent years the SHSG technique has improved with the introduction of new contrast media, 3D ultrasound, use of color Doppler and better ultrasound resolution. At present, it seems that SHSG can replace HSG as the first-line method in the study of infertility, one of its main advantages being the direct and dynamic examination of the fallopian tubes.
What advantages does virtual hysterosalpingography have over conventional hysterosalpingography?
Virtual hysterosalpingography allows a more complete diagnosis to be made because much more detailed images are obtained, both of the interior and the walls of the organs. It also makes it possible to obtain information on other organs located in the pelvis, apart from the uterus and the tubes, and can create three-dimensional images.
In addition, it causes less discomfort to the woman and the risks associated with iodinated contrast and radiation are also lower.
Recommended readings
A female fertility study is composed of several tests, including hysterosalpingography. You can learn all the details about each of the tests in the following article: Fertility tests in women.
In addition, if you want to know more information about the possible reasons for infertility in women, you can visit this article: What causes female infertility & sterility? Symptoms and treatments.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Al-Badawi IA, Fluker MR, Bebbington MW. Diagnostic laparoscopy in infertile women with normal hysterosalpingograms. J Reprod Med 1999; 44:953-7.
Gaurav S Desai. Virtual Hysterosalpingography: Its Place in the Workup of Infertile Women. J Obstet Gynaecol India. 2015 May;65(3):206-8. doi: 10.1007/s13224-015-0702-0. Epub 2015 May 3 (View)
Hemashree Rajesh, Serene Liqing Lim, Su Ling Yu. Hysterosalpingo-foam sonography: patient selection and perspectives. Int J Womens Health. 2016 Dec 28:9:23-32. doi: 10.2147/IJWH.S123710 (View)
Mol BW, Collins JA, Burrows EA, van der Veen F, Bossuyt PM. Comparison of hysterosalpingography and laparoscopy in predicting fertility outcome. Hum Reprod 1999;14:1237-42 (View)
Patricia Carrascosa, Carolina Sueldo, Carlos Capuñay, Mariano Baronio, Sergio Papier. Virtual hysterosalpingography in the diagnosis of bicornuate versus septate uterus. Fertil Steril. 2011 Nov;96(5):1190-2. doi: 10.1016/j.fertnstert.2011.08.026. Epub 2011 Sep 25 (View)
Zining Xu Yaoting Wang, Juan Sun, Shuangxi Chen, Zou Yan, Chen Lin, Jing Shu. Evaluation of tubal patency by hysterosalpingo-contrast Sonography (HyCoSy): Controversies, dilemmas and considerations. Heliyon. 2023 Jun 28;9(7):e17461. doi: 10.1016/j.heliyon.2023.e17461 (View)
FAQs from users: 'What are the benefits of virtual hysterosalpingography?', 'What are the differences between hysterosalpingography and hysterosonosalpingography?' and 'What advantages does virtual hysterosalpingography have over conventional hysterosalpingography?'.
Authors and contributors

More information about Cristina Algarra Goosman