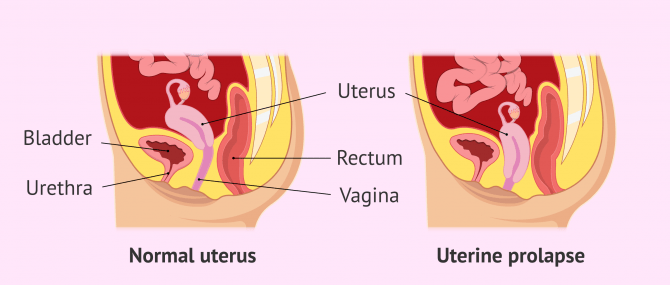
The uterus is held in the pelvis by muscles, ligaments, and other structures. If these tissues weaken, the uterus drops. Uterine prolapse is the displacement of the womb or uterus into the vaginal area.
Depending on the direction of uterine displacement, the prolapse will be anterior or posterior and will be called cystocele and rectocele respectively.
Generally, uterine prolapse does not require specific treatment unless the woman feels uncomfortable. In this case, the specialist will establish some advice and treatment and to help the patient so that she can lead a normal life.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 2.
- 3.
- 4.
- 4.1.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 6.
- 7.
- 8.
Definition of uterine prolapse
Uterine prolapse is the medical term used when there is a stretching of the pelvic floor ligaments, causing them to become weak. As a result, the uterus is no longer supported and falls into the vagina.
Uterine prolapse in women can occur at any age, although it is more likely in women who have had several vaginal births and have already reached menopause.
Both the diagnosis and treatment of uterine prolapse is complicated, as there are several reasons why it occurs. In addition, some symptoms experienced by some women with uterine prolapse are similar to clinical manifestations that arise in other conditions, further complicating diagnosis.
Symptoms
Most women with mild uterine prolapse do not notice any discomfort. If the uterine prolapse is moderate or severe, the most prominent symptoms are as follows:
- Urinary incontinence or sudden urge to urinate.
- Pain during sexual intercourse.
- Pressure in the vagina or pelvis.
- Lumbago.
- Repeated bladder infections.
- Vaginal bleeding.
- Increased vaginal discharge.
- Displacement of the uterus and cervix into the vagina.
In more serious cases, complications such as infections, ulceration of the cervix and vaginal walls, etc. can arise.
These symptoms get worse when a woman sits or stands for long periods of time and also in the early morning hours.
When some of these symptoms become more intense or interfere with your daily routine, it is best to consult your doctor.
Why does uterine prolapse happen?
Uterine prolapse is fairly common in women who have had one or more vaginal births. In addition, factors such as aging, lack of estrogen at menopause, a pelvic tumor, and other conditions that put pressure on the pelvic muscles can also cause uterine prolapse.
Although these are the most common causes of uterine prolapse, they are not the only ones. Here are other risk factors that increase a woman's chance of developing uterine prolapse:
- Giving birth to a baby of great weight and length.
- Advanced age in women.
- Obesity.
- Prolonged constipation.
- Being of hispanic or white ethnicity.
- Chronic cough.
- Lifting heavy objects.
In any case, family history should not be forgotten. If connective tissue weakness runs in your family, it may be a risk factor for uterine prolapse.
Diagnosis
The first test to diagnose uterine prolapse in women is a pelvic exam. The doctor will ask the patient to push as if she was pushing the baby out during labor. This will show how far the uterus descends into the vagina:
- If the cervix goes down to the lower part of the vagina, uterine prolapse is mild.
- If the cervix drops down outside the vaginal opening, uterine prolapse is moderate.
In addition, the doctor may ask the patient to tense the pelvic muscles in the same way as if she were going to hold her urine. The specialist will then be able to assess the strength of the pelvic muscles.
Treatment
As we have already mentioned, treatment for uterine prolapse is only necessary if the symptoms cause discomfort for the woman and prevent her from carrying out her daily activities. Many women receive it when the uterus has dropped down to the opening of the vagina.
Lifestyle changes such as losing weight or avoiding exertion can help control the symptoms associated with uterine prolapse.
On the other hand, another recommended therapeutic measure is a screw-shaped device, called a pessary. This device is placed inside the vagina and holds the uterus in place.
Pessaries must be cleaned regularly and may have some side effects such as foul-smelling discharge, vaginal ulcers, or problems with sexual intercourse. If the symptoms are very severe, surgery may be used, including removal of the uterus. A vaginal hysterectomy is often performed.
Prevention
Some of the measures that can help women avoid uterine prolapse are:
- Do daily Kegel exercises, especially after before and after childbirth. These exercises help strengthen the pelvic floor muscles.
- Avoid constipation by eating a balanced diet rich in fiber and drinking plenty of fluids.
- Lifting heavy objects correctly.
- Lead an appropriate lifestyle to avoid weight gain.
On the other hand, not smoking and avoiding polluted areas to avoid coughing also help in the prevention of uterine prolapse.
FAQs from users
Does uterine prolapse affect pregnancy?
Genital prolapse is the exit or herniation of one or more pelvic organs through the vaginal wall and external genitalia. Its frequency in reproductive ages is lower, since it is usually a more common pathology in menopause. Risk factors have been widely recognized as possible causes: multiparity, obstetric trauma, prolonged expulsive periods, obesity, sacro-nervous lesions, chronic pneumopathies, estrogen deficiency, etc.
Uterine prolapse in a young woman coinciding with pregnancy is an almost exceptional occurrence since only 233 cases had been reported up to 1968. Most of the cases reported in the literature occurred in the years prior to 1970, so that the modernization of obstetrics in recent years has made this situation even rarer today.

The main complications of uterine prolapse during pregnancy are miscarriage (15-21%), threatened preterm labor (18%), pelvic pain, leucorrhea, uterine incarceration, urinary retention, and increased urinary tract infections.
How do I know if I have uterine prolapse? What are the symptoms?
Uterine prolapse is the dropping of the uterus through the vagina, due to an alteration in the systems that hold the uterus to the pelvic wall (failure of ligaments and other supporting elements). Normally, the patient perceives a lump in the genitals that can be reduced with manual pressure.
It is important to differentiate it from bladder prolapse (descent of the bladder through the vagina) and rectal prolapse (descent of the rectum through the vagina). All of them together are called pelvic organ prolapse.
The main factor in triggering pelvic organ prolapse is previous vaginal delivery (especially instrumental delivery). In any case, all of them are susceptible to surgical intervention if a degree of descent is reached that affects the patient's quality of life, since it is a benign pathology.
What is colpocleisis?
Colpoclesis is a surgical way to treat uterine prolapse. This intervention consists of joining the anterior and posterior walls of the vagina, preventing them from protruding outward.
This treatment option for uterine prolapse is only recommended for women who are not sexually active, since colpoclesis closes the vaginal canal.
The success rate of colpocleisis is approximately 90-95%, although it will depend on the situation of each woman.
Are uterine prolapse and vaginal prolapse the same thing?
No. Uterine prolapse and vaginal prolapse are two different types of prolapse, although they are sometimes used synonymously.
Uterine prolapse is characterized by the uterus dropping into the vagina. In contrast, vaginal prolapse usually occurs in women who do not have a uterus and what happens is that the vagina is turned inside out.
Suggested for you
One of the main reasons why uterine prolapse can occur is the onset of menopause. Read here if you want to learn more about the final stage of a woman's menstrual cycle: Menopause in women: when it occurs and what symptoms it has.
We also have mentioned that it is sometimes necessary to resort to hysterectomy or removal of the uterus as a treatment for prolapse. In these cases, surrogacy will be necessary to achieve a pregnancy. In this link, you can read all the information related to this topic: What is surrogacy - Definition, types and indications.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Authors and contributors






I have actually been gone for quite a while, fortunately I recall exactly why I used to really enjoy your blog. Thank you very much, I will make sure to check back again. How many times you up-date your web page?