Choosing the gender of babies, whom are commonly referred to as designer babies, has been the subject of extensive debate within the field of assisted reproductive technology (ART) from its beginning.
From a scientific point of view, it is now possible for prospective parents to conceive a girl or a boy by choosing the sex of their baby with certain methods, thanks to the recent advancements in fertility treatments. However, the truth is that selecting the gender of the baby, also known as family balancing, does not increase the chances of getting pregnant in any way.
In some countries, gender selection is permitted only with the purpose of preventing the transmission of sex-linked genetic diseases. In other countries, such as the United States, gender selection for family balancing is a common practice among fertility clinics.
Provided below is an index with the 8 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 5.4.
- 5.5.
- 6.
- 7.
- 8.
What is gender selection?
During embryo development, sexual differentiation occurs before fertilization and is determined by the genetic material contributed by the sperm of the father, that is, the father's genes are responsible for the child's sex. Sperm cells carry either X or Y sex chromosomes. Given that egg cells always have an X chromosome, two combinations are possible:
- If the sperm carries an X-chromosome the baby will be XX, a girl.
- If the sperm carries a Y-chromosome the baby will be XY, a boy.
In this sense, gender selection involves the manipulation of the early stages of fertilization or embryonic development to have a child of the desired sex, whether male or female.
Assisted reproduction techniques allow us to choose the gender of the baby in any of the following stages:
- Before conception
- It involves choosing the sperm of the desired gender before fertilization, which allows us to do it without IVF.
- After conception
- The embryo of the desired gender is selected right after fertilization and transferred back to the mother's uterus.
- During pregnancy
- The woman decides to terminate the pregnancy voluntarily should she be pregnant with a baby of the undesired sex. It is known as sex-selective abortion.
For ethical reasons, sex-selective abortion is not a recommended technique for choosing the sex of unborn babies. However, a woman is free to opt for voluntary termination of pregnancy (VTP or VTOP). All in all, it is a matter of choice.
Pre-selecting the gender of a baby has a series of pros and cons that are listed in the following sections:
Advantages
The following are the most common arguments given by those in favor of selecting the sex of their baby:
- It is an opportunity for would-be parents to limit the size of their family, which makes it easier for them to take care of the kids.
- It helps to prevent the transmission of gender-related diseases to offspring.
- Some proponents believe that parents are more loving if they have a child with a gender they prefer.
- If a couple have lost a child, having a baby with the same gender can help get over the loss.
Disadvantages
On the other side of the coin, the following are the arguments of those who are against sex selection:
- It is expensive and actually unnecessary, as does not increase the likelihood of getting pregnant.
- One of the funniest things for a couple during pregnancy is guessing the gender of their baby. If they choose it before or after conception, the element of surprise is eliminated.
- It is not 100% accurate, unless the technique of choice is IVF with PGD for gender selection, which offers 100% but is the most expensive option.
- It contributes to gender inequality and may lead to a population imbalance.
Before conception: sperm sorting
As mentioned earlier, the methods included in this group are used for sperm sorting, that is, choosing the sperm that carries the Y- or X-chromosome as desired.
The main advantage of sperm sorting is that creating excess embryos is not required. On the other hand, this group of techniques do not offer very accurate outcomes, and for this reason their use by fertility specialists has declined in recent years.
The most common options are explained in the following sections:
MicroSort technique
This high-tech method focuses on the genes contained inside the sperms cells.
The guiding principle of this technique is that the Y-chromosome is smaller in size than the X-chromosome. Keeping this in mind, the male sperm contain 2.8% less DNA inside than the female sperm.
The device used to distinguish between male and female spermatozoa is called flow cytometer or cell sorter, and the technique is known as MicroSort.
After separating the sperms carrying the X chromosome from the ones that carry the Y chromosome, they can be put into the female reproductive tract by means of intrauterine insemination (IUI) to achieve a pregnancy.
The accuracy rate of MicroSort is 70-80%. However, it is still being studied in clinical trials, and has not been approved by the Food and Drug Administration (FDA) in the USA because it involves staining the sperm with a fluorescent dye that could compromise the viability of the sperm after the procedure.
Ericsson or sperm spinning method
This technique is based on the "swimming" speed of spermatozoa.
Taking into account the amount of ADN each sperm carries, it is believed that those carrying the Y-chromosome are faster and lighter than those carrying the X-chromosome, which are slower swimmers.
By modifying the protocol followed for sperm washing (sperm capacitation) in the laboratory, we can enrich the semen sample with the sperms of the desired gender, and place them directly in the uterus of the intended mother by means of IUI.
The success rate of the Ericsson method is 70% approximately.
Shettles method
It involves timing intercourse so that it takes place while the woman is on the fertile window of her menstrual cycle.
Proponents of the Shettles method support the belief that sperms carrying the Y-chromosome are faster yet have a shorter lifespan than X-chromosome spermatozoa. This means that, during the days prior to ovulation, the chances for becoming pregnant with a boy are higher. Conversely, if intercourse occurs four or five days before ovulation, chances are that the woman will get pregnant with a girl, as X-chromosome sperms live longer.
It is possible for women to determine when ovulation is going to take place by charting their basal body temperature (BBT).
Some experts who are in favor of this theory consider that it has a 75% accuracy rate. It has been broadly questioned by others, though.
Whelan method
It consists in timing intercourse in accordance with the moment of ovulation as well. However, this technique is inconsistent with the Shettles method, which we have just explained above.
According to this theory, the biochemical changes that make it easier for the Y-chromosome sperms to fertilize the egg occur during the early stages of the menstrual cycle. So, if the desired gender is male, intercourse should occur between 4 to 6 days prior to ovulation. On the other hand, if it takes place 2-3 days before the woman ovulates, the chances are that she gets pregnant with a girl.
The accuracy of this method has been as broadly questioned as that of the Shettles method. Some state that it can be 60% accurate, though.
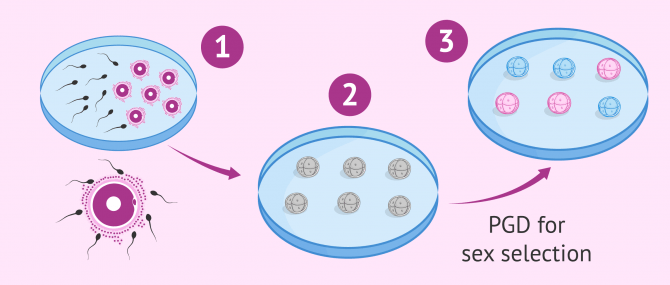
After conception: IVF with PGD
The abbreviation PGD stands for Preimplantation Genetic Diagnosis, a technique that is performed once the embryos have been obtained in the laboratory by means of in vitro fertilization (IVF).
PGD is used mainly to select an embryo that is "genetically healthy", which is to say, to prevent the birth of offspring with genetic abnormalities. Given that this technique allows for the embryo's full set of chromosomes to be analyzed, it is possible for the specialist to also determine the presence of either the X- or the Y-chromosome, thereby guessing the sex of each embryo.
After this genetic test, the embryos selected can be transferred to the intended mother's womb with the purpose of achieving pregnancy.
It should be noted that PGD is a 100% accurate technique, both for gender selection and for the prevention of genetic abnormalities or diseases. Nevertheless, women over the age of 35 who are planning to get pregnant are strongly recommended to undergo an amniocentesis to rule out the presence of genetic alterations.
How much do sex selection methods cost?
In general, the price of sperm sorting methods ranges from $1,300 to $2,500 each attempt. These methods are widely practiced in US clinics, but their success rates reach up to 85%.
In the case of the MicroSort method, the cost is $3,400, but currently clinics are waiting for FDA approval, so clinics have stopped using it for the moment.
IVF with PGD for gender selection is, on the other hand, the most accurate method: programs with PGD for sex selection offer virtually 100% accuracy. However, it is the most expensive option, as it can add $3,000 or even $5,000 to the cost of IVF. On average, the total price is $14,000-25,000 per attempt.
As for insurance, most fertility clinics accept it for fertility treatment, but coverage for family-balancing procedures is uncommon. Those coping with infertility who, in doing so, want to choose the gender of their baby, may have part of it covered.
Considering seeing a fertility specialist? Don't forget that, in the field of Reproductive Medicine, as in any other medical area, it is crucial that patients rely on the doctors and staff that will help them through their treatment cycle. Logically, conditions vary from clinic to clinic. For this reason, we recommend that you generate your Fertility Report now. It will offer you a list of clinics that have passed our rigorous selection process successfully. Furthermore, the system will make a comparison between the fees and conditions of each clinic so that you can make a better-informed decision.
FAQs from users
Can you choose your baby’s gender in the USA?
In the USA, gender determination of the embryo is allowed and is easily performed through embryo biopsy then comprehensive chromosome screening called PGT-A (preimplantation genetic testing for aneuploidy).
The procedure involved the embryo(s) undergo removal of several outer cells followed by vitrification (freezing) while the cells are sent to a specialized laboratory to be analyzed. The entire chromosomal content of the embryo(s) is analyzed to in addition to determining the sex so the intended parent(s) received a chromosomally normal embryo of the desired gender.
Is IVF with gender selection possible?
Gender selection is possible through a procedure known as pre-implantation genetic diagnosis (PGD). Sex selection for social use is allowed in a small number of countries, though.
PGD is used for the genetic screening of the embryos before transferring them to ensure they are healthy, without chromosomal abnormalities, genetic disorders or birth defects.
It allows gender selection because the X and Y chromosomes have to be analyzed to dismiss the presence of sex chromosome abnormalities. At that point, the gender of each embryo (XX or XY) can be determined.
Are there any risks to the mother or the baby with of PGD for gender selection?
Firstly, there are no additional to women undergoing IVF but only those experienced by any other patient undergoing IVF, which include multiple pregnancy, ovarian hyperstimulation syndrome (OHSS), pelvic infections, internal bleeding during egg collection, ectopic pregnancy, etc.
Secondly, as regards the baby, available data shows that pregnancy rates are reduced with each cell that is removed from the embryo for PGD testing. However, practical experience does not support this indications. Nowadays, embryologists remove a single cell from the embryo, so there is no reason to worry about.
Which genetic diseases can be prevented with PGD for gender selection?
Recessive genetic disorders linked to the X-chromosome such as Duchenne muscular dystrophy (DMD), hemophilia, color blindness, fragile X syndrome (FXS), etc.
It is also possible to prevent certain diseases associated with the Y-chromosome, including but not limited to, azoospermia factor (AZF) microdeletions.
What are the ASRM's guidelines regarding gender selection?
The Ethics Committee for the American Society for Reproductive Medicine (ASRM) has established the following guidelines:
Physicians should be free to offer preconception gender selection [...] if the couples 1) are fully informed of the risks of failure, 2) affirm that they will fully accept children of the opposite sex, if the preconception gender selection fails, 3) are counseled about having unrealistic expectations [...], and 4) are offered the opportunity to participate in research to track and assess the safety, efficacy and demographics of preconception selection.
Suggested for you
In order to select the gender of the baby, undergoing fertility treatment is a pre-requisite. If you want to learn more about the different infertility treatment options available nowadays, do not miss the following post: Guide to infertility treatments.
The fact that sex selection is forbidden in many countries has promote the so-called fertility tourism or reproductive tourism. Would you like to learn more about this phenomenon? Visit this post: IVF abroad: options and main benefits.
Finally, in case you are interested in PGD for gender selection and would like to learn the details about this technique, you can do so by reading this guide: What is Preimplantation Genetic Diagnosis or PGD?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
FAQs from users: 'Can you choose your baby’s gender in the USA?', 'Is IVF with gender selection possible?', 'Are there any risks to the mother or the baby with of PGD for gender selection?', 'Which genetic diseases can be prevented with PGD for gender selection?' and 'What are the ASRM's guidelines regarding gender selection?'.





Hello Sandra,
We’re considering gender selection but with our frozen embryos… our RE said it is possible and the main advantage of doing it with frozen embryos is that it can be done after freezing. Our question is if it will reduce the survival potential of the embryo post thaw…
Thank you for your help!
Hello Ciara_ON,
If the biopsy is done on Day 5, the risk that the embryo is not able to survive is minimal. That’s why clinics do it on Day 5 on a regular basis nowadays. Do not worry about this.
I hope I have been able to help,
Best wishes